Nature:研究揭示肝细胞再生新机制!
2017-08-26 枫丹白露 来宝网
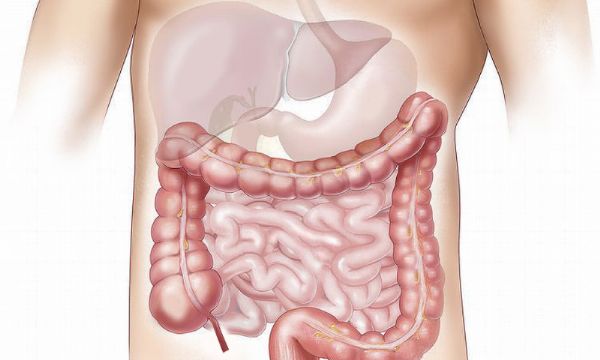
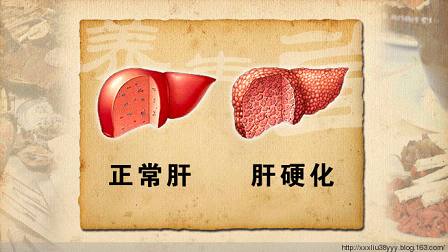
国际研究协作首次证明胆管细胞(上皮胆管细胞)在肝脏再生中的作用。研究结果对再生医学和抗击肝病具有重要意义。该团队的发现已发表在“自然”杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肝细胞#
57
#肝细胞再生#
64
#Nat#
84
还好还好哈几号聚
78