盘点:近期短暂性脑缺血研究进展一览
2016-09-29 MedSci MedSci原创
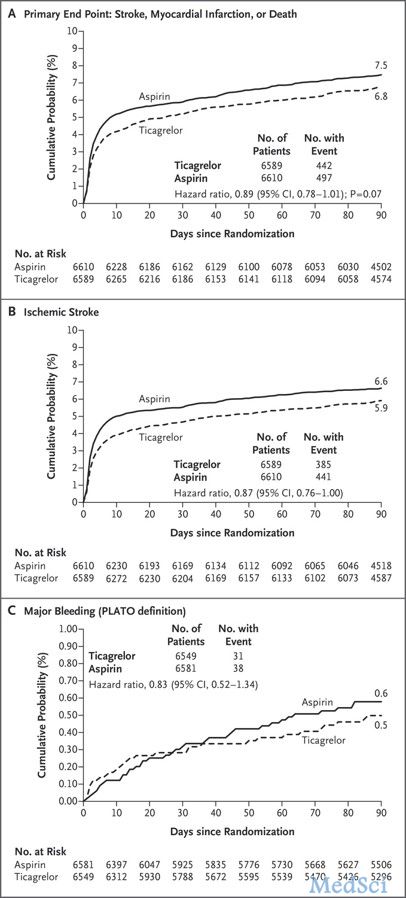
短暂性脑缺血发作(Transient ischemic attack,TIA)是脑、脊髓或视网膜局灶性缺血所致的、未发生急性脑梗死的短暂性神经功能障碍,TIA与缺血性卒中有着密不可分的联系,大量研究显示,TIA患者在近期有很高的卒中发生风险。2010年我国TIA流行病学调查显示,我国成人标化的TIA患病率为2.27%,知晓率仅为3.08%,在整TIA人群中,有5.02%的人接受了治疗,仅4.0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










测试测试
61
#短暂性#
60
#短暂性脑缺#
88
学习了,多谢分享!
90
学习了,多谢分享!
87
学习了,多谢分享!
94
继续关注
74
继续学习
90
#脑缺血#
60
#研究进展#
56