ANN THORAC SURG:一例同时侵犯左右心房的原发性心脏嗜铬细胞瘤
2013-01-10 刘兴荣 等 MedSci原创 Peter译
嗜铬细胞瘤是来源于神经嵴的产生儿茶酚胺的肿瘤。原发性心脏嗜铬细胞瘤是极为罕见的,全世界目前见于文献报道的仅为100例左右,北京协和医院心外科去年1月份成功进行了一例心脏嗜铬细胞瘤切除手术,患者为中年女性,肿瘤同时侵犯左右心房,其MIBG闪烁扫描的结果正常,但奥曲肽显像结果异常。肿瘤在体外循环下被成功切除。该病例报告已经发表在著名心胸外科专业杂志Annals of Thoracic Surgery上

Fig 1. (A) 99m-Technetium-labeled hydrazinonicotinyl-Tyr3-octretide scintiscan demonstrated a focus of intense uptake on right side of heart silhouette. (B) Contrast-enhanced computed tomographic scan illustrated tumor (arrow) overlying interatrial groove. (LA = left atrium; RA = right atrium.)
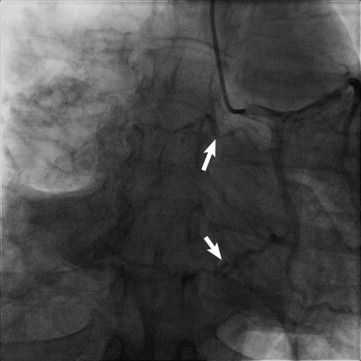
Fig 2. Coronary angiogram demonstrated a tumor blush with 2 feeding vessels (white arrows) branching from left circumflex artery.

Fig 3. Resected cardiac pheochromocytoma.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#THORAC#
0
#右心房#
82
#原发性#
66
#细胞瘤#
58
#心房#
62
协和V5
91