JCEM: 研究显示糖尿病合并慢性胰腺炎并发症风险加倍
2020-03-13 国际糖尿病 网络
糖尿病是以胰岛素抵抗和分泌不足为特征的进行性代谢疾病,慢性胰腺炎是胰腺逐渐纤维化进而胰腺内分泌及外分泌功能逐渐丧失的进展性炎症疾病。当二者合并存在,会对健康带来怎样的影响?近日,发表于《临床内分泌与代
糖尿病是以胰岛素抵抗和分泌不足为特征的进行性代谢疾病,慢性胰腺炎是胰腺逐渐纤维化进而胰腺内分泌及外分泌功能逐渐丧失的进展性炎症疾病。当二者合并存在,会对健康带来怎样的影响?近日,发表于《临床内分泌与代谢杂志》的一项基于中国台湾人群的研究结果显示,糖尿病合并慢性胰腺炎可进一步增加严重并发症的风险,如糖尿病酮症酸中毒(DKA)、高血糖高渗状态和低血糖。

这项队列研究以1999~2010年506例新诊断慢性胰腺炎(CP)且合并糖尿病成人患者为研究队列,同时以5060例年龄和性别相匹配且同期没有慢性胰腺炎的糖尿病患者作为对照队列。主要观察指标为DKA、高血糖高渗状态、低血糖事件发生率和死亡率。
糖尿病合并慢性胰腺炎并发症风险更高
研究队列(糖尿病合并慢性胰腺炎)中以男性(88.9%)为主,以中青年居多(<45岁:60.08%,45~64岁:32.02%,≥65岁:7.90%)。与对照队列相比,研究队列中受试者合并症更多,包括CKD、肝病、酒精中毒、胆石症、尿路感染和肺炎;糖尿病相关并发症也更多(aDCSI评分更高)(P=0.026)。
研究队列中,DKA1年、5年和10年累积发生率分别为2.2%、11.1%和14.4%,对照队列中分别为0.3%、1.1%和1.8%,研究队列中受试者发生DKA风险高出对照队列9.5倍(95%CI,6.51~13.91,P<0.0001),见图1。
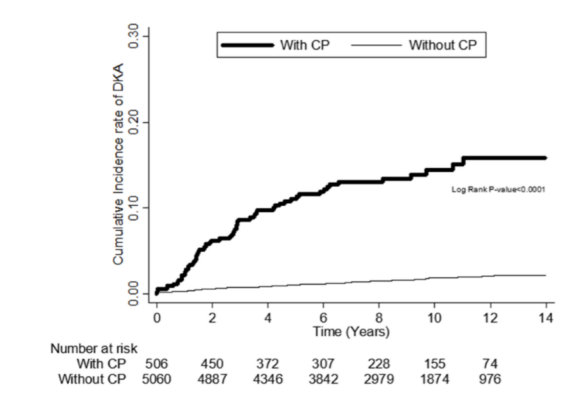
图1. 糖尿病合并慢性胰腺炎患者DKA发生率高于单纯糖尿病患者
研究队列中,高血糖高渗状态1年、5年和10年累积发生率分别为1.2%、5.3%和7.1%,对照队列中分别为0.2%、0.7%和1.1%,研究队列中受试者发生高血糖高渗状态风险高出对照队列4.96倍(95%CI,2.85-8.62,P<0.0001),见图2。
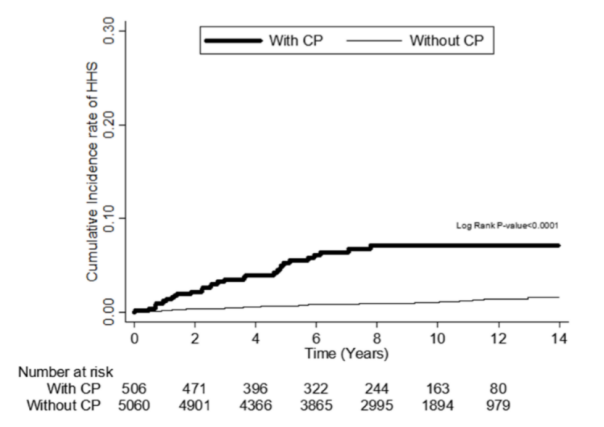
图2 糖尿病合并慢性胰腺炎高血糖高渗状态发生率高于单纯糖尿病患者
研究队列中,低血糖1年、5年和10年累积发生率分别为2.4%、10.5%和21.1%,对照队列中分别为0.7%、3.1%和5.6%,研究队列中受试者发生低血糖风险高出对照队列3.02倍(95%CI,2.23-4.08,P<0.0001)。见图3。
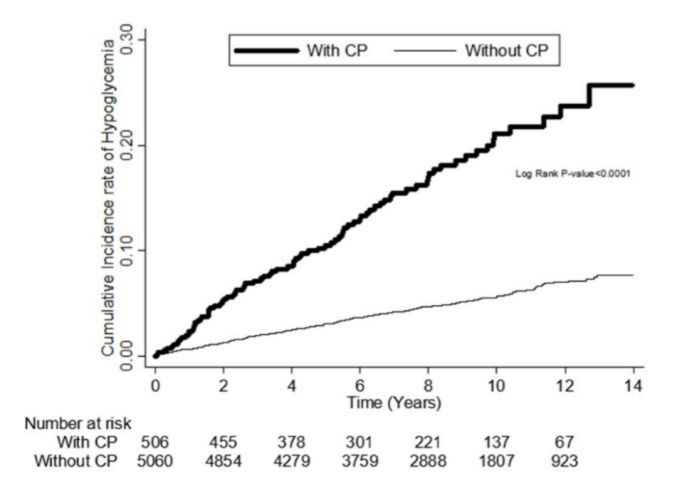
图3 糖尿病合并慢性胰腺炎患者低血糖发生率高于单纯糖尿病患者
糖尿病合并慢性胰腺炎全因死亡率升高2.43倍
研究队列中受试者全因死亡率为23.88‰,对照队列中为6.87‰。在对其他共病进行调整后,研究队列中受试者的死亡风险高出对照队列的2.43倍(95%CI,1.82-3.27,P<0.0001)。见图4。
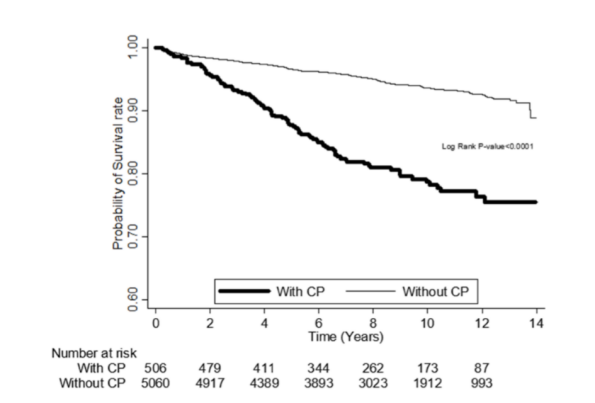
图4 糖尿病合并慢性胰腺炎患者全因死亡率高于单纯糖尿病患者
此项研究结果显示,糖尿病合并慢性胰腺炎发生急性并发症风险显著增加,包括DKA、高血糖高渗状态、低血糖和死亡。目前已分析其间的相关性,还需进一步研究以明确因果关系。同时,需要更加密切地关注这一人群的血糖管理和降糖药物的使用情况。
中国台湾台南智美医疗中心肾内科副教授Chih-Chiang Chien表示:“糖尿病合并慢性胰腺炎患者发生DKA、高血糖高渗状态和低血糖的风险分别高于单纯糖尿病患者的9.5倍、5倍和3倍。建议糖尿病患者避免饮酒,有胆道疾病者尽早治疗,定期监测血脂水平,以避免慢性胰腺炎的发生。对于合并慢性胰腺炎的糖尿病患者,应预防高血糖危象和低血糖。“
原始出处:
LinCH,etal.Effect of Chronic Pancreatitis on Complications and Mortality in DM Patients: A 10-year Nationwide Cohort Study. JClinEndocrinolMetab.2020;doi:10.1210/clinem/dgaa035.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










受教了
96
#JCE#
65
#JCEM#
57
#并发#
93
糖尿病和胰腺癌也有相关性
140
谢谢MedSci提供最新的资讯
68
學習了,很有用,不錯
106