Ophthalmic Plast Reconstr Surg:侵入眼眶的结膜性假腺瘤增生
2018-07-24 cuiguizhong MedSci原创
纽约大学Langone医学中心眼科和病理学系的Charles NC近日在Ophthalmic Plast Reconstr Surg发表一篇病例报告,他们在一例患者中发现侵入眼眶的结膜性假腺瘤增生。
纽约大学Langone医学中心眼科和病理学系的Charles NC近日在Ophthalmic Plast Reconstr Surg发表一篇病例报告,他们在一例患者中发现侵入眼眶的结膜性假腺瘤增生。
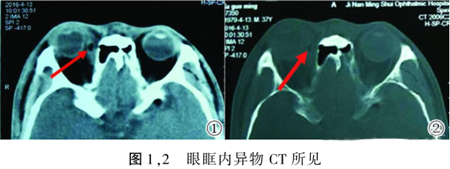
一名41岁的女性在上呼吸道感染后出现持续性单侧结膜炎。经计算机断层扫描发现,在穹窿部位出现白色囊性病变,并从眼眶后面延伸到眼眶的前部。在局部全切除后,组织病理学检查显示具有良性假腺瘤(假腺)增生。
作者认为,这个病例是该病变在结膜中发生的第五次报告,但是唯一一例进入眼眶的病例。
原文出处:
Charles, N.C. and R.N. Palu, Orbital Extension of Conjunctival Pseudoadenomatous Hyperplasia. Ophthalmic Plast Reconstr Surg, 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AST#
48
#NST#
62
#THA#
60
#眼眶#
64
学习了,获益匪浅,感谢分享
79
学习了
96
很好的学习机会
106