实际问题:放了支架,还能做磁共振吗?
2015-04-22 佚名 介入家园
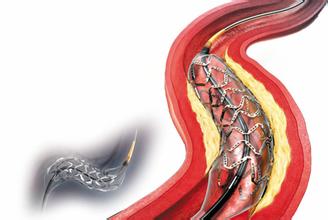
随着介入治疗技术普及,心脏支架,颅内支架,大动脉支架、食管胆道支架等各种各样的支架越来越多地出现在临床工作中,而随之而来的问题是:放了支架后,还能做磁共振吗?毕竟磁共振是当前非常重要的一种检查手段,如果不能够做磁共振的话,将会影响很多疾病的诊断。不光是支架,现在介入治疗中还会使用很多的人体植入物,如:弹簧圈、滤器、动脉夹及人造血管等等。这些做磁共振会有影响吗?我们的教材上没有答案,为此,小编查阅了
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











。
121
。
112
#磁共振#
55
了解
152
顿悟
156
谢谢分享,起搏器自己IABP仍然是绝对是禁忌症
140
保险起见 最好避免
111