Eur Heart J:欧洲心脏杂志刊登深圳医生病例,小血管闭塞,也引发大灾难
2018-11-23 文韬 中国循环杂志
室间隔穿孔几乎都是大冠状动脉病变导致的,而这是第一例单纯间隔支闭塞引发心脏破裂的首次报告,该病例通过使用经皮封堵治疗成功。
作者称,室间隔穿孔几乎都是大冠状动脉病变导致的,而这是第一例单纯间隔支闭塞引发心脏破裂的首次报告,该病例通过使用经皮封堵治疗成功。
一名65岁男士患有3天来呼吸困难、心悸。
入院血压偏低,92/60 mmHg,并有心动过速。
心电图显示V1-4导联的ST段抬高。肌钙蛋白轻度升高。
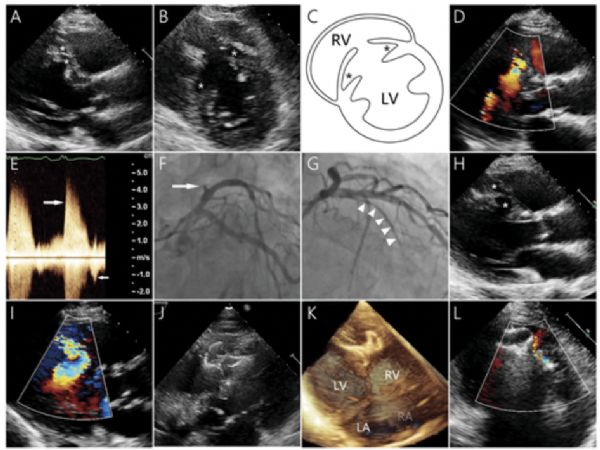
超声心动图显示室间隔穿孔,左右心室孔的最大直径分别为2.1 cm和0.8 cm。
彩色多普勒显示左右心室之间的双向分流(图D和E)。左心室没有室壁运动异常,射血分数约为70%。
冠状动脉造影显示,第一间隔支完全闭塞(图F),通过球囊血管成形术(图G)成功治疗,在左前降支中远段有中等程度病变。
入院后,患者病情恶化,复查超声心动图示破裂增大(图H和I)。
随后使用了静脉注射药物和主动脉内球囊泵进行稳定。
入院后2个月,使用1618 mm HeartR™封堵器(LifeTech Scientific Corporation,深圳,中国)进行了经皮封堵缺损,术后有小的残余分流(图J-L)。
在6个月的随访中,病人无症状。
原始出处:
Xinbo Zhong Guili Zhou Zhifu Huan, et al. Small septal vessel occlusion results in big damage: ventricular septal dissection and rupture. European Heart Journal, Volume 39, Issue 26, 7 July 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#血管闭塞#
64
#欧洲#
47
#ART#
56
#HEART#
47
临床上很少见到这类病人
74
学习了很有用
76