ASCO2022:纳武利尤单抗能显著增加高危肌层浸润性尿路上皮癌患者无病生存时间
2022-06-01 MedSci原创 MedSci原创
在CheckMate 274试验中,纳武利尤单抗(NIVO)与安慰剂(PBO)相比,无论在有意治疗(ITT)的患者(pts)( HR=0.70;98.22% CI,0.55-0.90;P<0.001)
在CheckMate 274试验中,纳武利尤单抗(NIVO)与安慰剂(PBO)相比,无论在有意治疗(ITT)的患者(pts)( HR=0.70;98.22% CI,0.55-0.90;P<0.001)还是在肿瘤程序性死亡配体1(PD-L1)表达≥1%的患者(HR=0.55;98.72%CI,0.35-0.85;P<0.001),无病生存(DFS)得到了显著改善。
近期,来自荷兰的学者在ASCO2022报告了最主要的尿路上皮癌类型膀胱癌患者亚组的结果。CheckMate 274是一项3期随机双盲试验,对根治性切除后的高危肌层浸润性尿路上皮癌(膀胱、输尿管、肾盂)进行NIVO与PBO辅助治疗。患者按1:1的比例随机接受NIVO 240毫克静脉注射,每2周一次或PBO,辅助治疗时间≤1年,并按结节状态、先前新辅助顺铂和肿瘤PD-L1表达进行分层。患者接受了根治性切除术±新辅助化疗,并在最终病理分期时有复发的高风险。主要终点是ITT患者和PD-L1≥1%的患者的DFS。次要终点为非尿道复发生存率(NUTRFS)。
在试验中的709名随机患者中,560名患有MIBC(NIVO,n = 279;PBO,n = 281)。至少随访11.0个月,总的来说,在这些患者中观察到NIVO与PBO的DFS效益。在所有MIBC患者中,NIVO的12个月DFS概率为66%,PBO为45%。根据年龄、性别、ECOG表现状态、结节状态和PD-L1表达状态,NIVO与PBO在各亚组中的DFS均有改善。
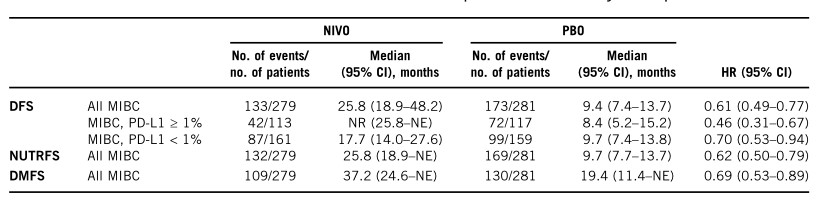
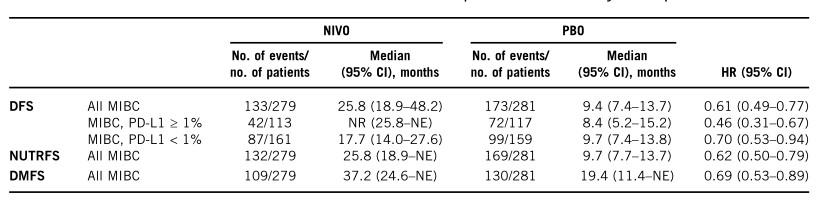
同时,还观察到NIVO与PBO的NUTRFS和DMFS的改善。在NIVO和PBO治疗组中,分别有17%和6%的患者发生3-4级治疗相关不良事件。
在根治性切除术后的MIBC患者中,无论肿瘤PD-L1表达情况如何,NIVO都比PBO观察到DFS的改善。
参考文献:
Results for patients with muscle-invasive bladder cancer (MIBC) in the CheckMate 274 trial. First Author: Alfred Alfred Witjes, Radboud University, Nijmegen, Netherlands
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#生存时间#
59
#ASC#
0
#上皮癌#
59