J Heart Lung Transplant:慢性血栓性肺动脉高压患者改善右室功能可选择球囊肺动脉成形术
2015-10-31 phylis 译 MedSci原创
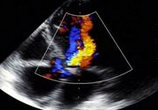
背景:慢性血栓性肺动脉高压(CTEPH)致右心室(RV)适应性改变,常致RV衰竭及死亡。球囊肺动脉成形术(BPA)是肺动脉内膜切除术禁忌及肺动脉内膜切除术后残余肺动脉高压患者的一种治疗方法。研究者假设CTEPH患者BPA后RV重塑逆转机改善RV功能。方法:26个CTEPH患者(59 ± 12岁,11个男性患者),在进行前后4±2 BPA进行超声心动图,心肺运动实验,血液样本及右心导管的检查。根据当
背景:慢性血栓性肺动脉高压(CTEPH)致右心室(RV)适应性改变,常致RV衰竭及死亡。球囊肺动脉成形术(BPA)是肺动脉内膜切除术禁忌及肺动脉内膜切除术后残余肺动脉高压患者的一种治疗方法。研究者假设CTEPH患者BPA后RV重塑逆转机改善RV功能。
方法:26个CTEPH患者(59 ± 12岁,11个男性患者),在进行前后4±2 BPA进行超声心动图,心肺运动实验,血液样本及右心导管的检查。根据当前指南,线下分析超声心动图RV的功能状态。应用成对t检验分析基线到随访期间的差异。
结果:BPA后血流动力学,耗氧量峰值及B型钠尿肽显著升高。RV功能改善,包括面积变化分数(+6%),三尖瓣收缩期移位(+3 mm)及右室游离壁峰值应变(-4.4)。右室舒张末期内径,面积,及游离壁厚度明显降低,而左室内径及每搏量增加。
结论:BPA后,超声心动图显示RV功能显著改善,为CTEPH患者进行BPA治疗增加了可信度。
原文出处:
Broch K, Murbraech K, Ragnarsson A, et al. Echocardiographic evidence of right ventricular functional improvement after balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension. J Heart Lung Transplant. 2015,Sep 3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血栓性#
63
#Transplant#
95
#成形术#
79
#TRA#
71
#plant#
73
#肺动脉高压患者#
70
#动脉高压#
72
#ART#
54
#球囊#
59
#HEART#
116