GUT:内窥镜下黏膜治疗不同方法的优势比较!
2017-10-15 MedSci MedSci原创
近期,一项发表在杂志gut上的研究旨在比较用于切除大于20mm的大的无蒂横向扩张的结肠直肠病变(LSL)的内窥镜粘膜下剥离术(ESD)和大面积内窥镜粘膜切除术(WF-EMR)的成本效益。此项研究在为期18个月的时间内使用决策树模型进行了增量成本效益分析。比较了以下策略:使用WF-EMR,通用ESD(U-ESD)和选择性ESD(S-ESD)用于含有粘膜下侵袭性癌症(SMIC)的高度可疑的病变,其余病
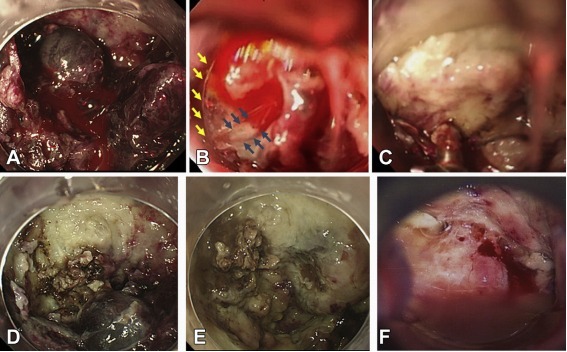
近期,一项发表在杂志gut上的研究旨在比较用于切除大于20mm的大的无蒂横向扩张的结肠直肠病变(LSL)的内窥镜粘膜下剥离术(ESD)和大面积内窥镜粘膜切除术(WF-EMR)的成本效益。
此项研究在为期18个月的时间内使用决策树模型进行了增量成本效益分析。比较了以下策略:使用WF-EMR,通用ESD(U-ESD)和选择性ESD(S-ESD)用于含有粘膜下侵袭性癌症(SMIC)的高度可疑的病变,其余病变使用WF-EMR。来自大型西方队列和文献的数据用于模型分析。有效性定义为每1000例患者中避免手术的次数。同时提出了避免手术的增量成本并进行了灵敏度和情景分析。
最终,此项研究共分析1765例患者中的1723例病变。SMIC和低分险SMIC的流行率分别为8.2%和3.1%。SMIC内镜病变评估的灵敏度和特异度分别为34.9%和98.4%。 S-ESD是最便宜的策略,并且通过每1000例病例预防19次额外手术也证明了其比WF-EMR更有效。在S-ESD战略中,需要采取43项ESD程序。 与S-ESD相比,U-ESD可以预防额外的13次手术,这些手术的增量成本为210112美元。在高风险直肠病变中,U-ESD只具有成本效益。
此项研究结果表明:S-ESD是首选治疗策略。但是,每1000个LSL只需要43个ESD。WF-EMR对大多数LSL仍然是一个有效和安全的治疗选择。
原始出处:
Bahin FF, Heitman SJ, et al. Wide-field endoscopic mucosal resection versus endoscopic submucosal dissection for laterally spreading colorectal lesions: a cost-effectiveness analysis. Gut. 2017 Oct 7. pii: gutjnl-2017-313823. doi: 10.1136/gutjnl-2017-313823.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#内窥镜#
77
#黏膜#
88
#优势比#
65
学习了.谢谢分享.
94