心电图学上“拦路虎”——房室阻滞,这篇文章你不可不读!
2022-02-16 心希望快迅 心希望快迅
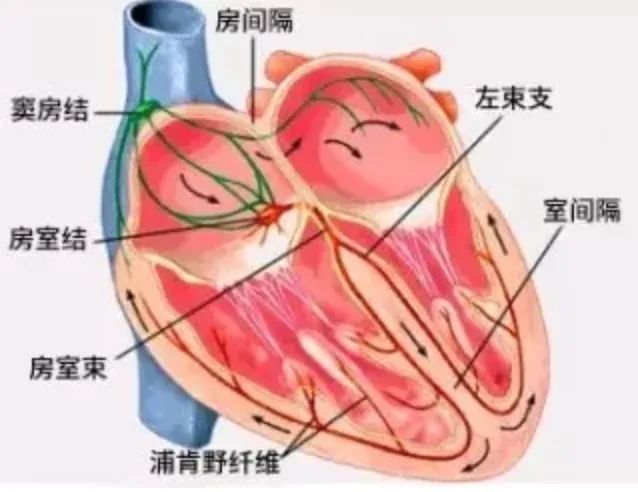
房室阻滞是指房室交界区脱离了生理不应期后,心房冲动传导延迟或不能传导至心室。可发生在房室结、希氏束及束支系统等不同部位。
房室阻滞是指房室交界区脱离了生理不应期后,心房冲动传导延迟或不能传导至心室。可发生在房室结、希氏束及束支系统等不同部位。
分为不完全性和完全性两类,前者包括一度和二度房室阻滞,后者又称三度房室阻滞。

(房室阻滞分类与发生部位和His束电图(HBE)及体表心电图(Ⅱ)的关系;图源:中国知网)
正常人可以出现一度房室阻滞,正常人或运动员可发生二度I型房室阻滞,与迷走神经张力增高有关,常为短暂性。其他导致房室阻滞的病变有:
①以各种原因的心肌炎最常见,如风湿性、病毒性心肌炎,心内膜炎等;
②各种器质性心脏病如冠心病、风湿性心脏病、心肌病及先天性心脏病等;
③洋地黄和其他抗心律失常药,如β受体阻滞药、维拉帕米、地尔硫卓、胺碘酮等,多数停药后,房室阻滞消失;
④电解质紊乱,如高血钾等;
⑤特发性的传导系统纤维化、退行性变等;
⑥心脏肿瘤、外伤及心脏外科手术时误伤或波及房室传导组织可引起房室阻滞。
一、临床表现
01 一度房室阻滞患者通常无症状。听诊时心尖部第一心音减弱。
02 二度房室阻滞患者可有心搏暂停感觉,心搏可变慢、不规律或两者都有,可能会引起心悸、乏力、心功能不全、头晕或晕厥等症状。听诊时可有第一心音减弱及心搏脱漏。
03 三度(完全性)房室阻滞时,心房至心室间冲动的传导被完全阻断,心脏另一部分组织充当起搏点以建立心室节律,较正常起搏点的心率慢,而且经常不规律、不可靠。因此,三度房室阻滞常导致疲倦、乏力、心绞痛、头晕或晕厥等症状,这取决于是否建立了心室自主节律及心室率和心肌的基本情况。自主节律点较高如恰位于希氏束下方,心室率较快达40~ 60次/min,患者可能无症状。双束支病变者心室自主节律点低,心室率慢在40次/min以下,可出现心功能不全和脑缺血综合征(adams-stokes syndrome,阿-斯综合征),患者可出现短暂性意识丧失甚至抽搐,严重者可猝死。如果心室自主节律未及时建立则出现心室停搏。心室率缓慢常引起收缩压升高和脉压增宽。三度房室阻滞的第一心音强度经常变化,不规则地出现响亮的第一心音。第二心音可有反常分裂。每搏量增大产生肺动脉瓣区收缩期喷射性杂音和第三心音。当心房与心室同时收缩时,颈静脉出现巨大a波。
二、心电图表现
01 一度房室阻滞心房至心室间冲动的传导被轻度延迟。表现为:
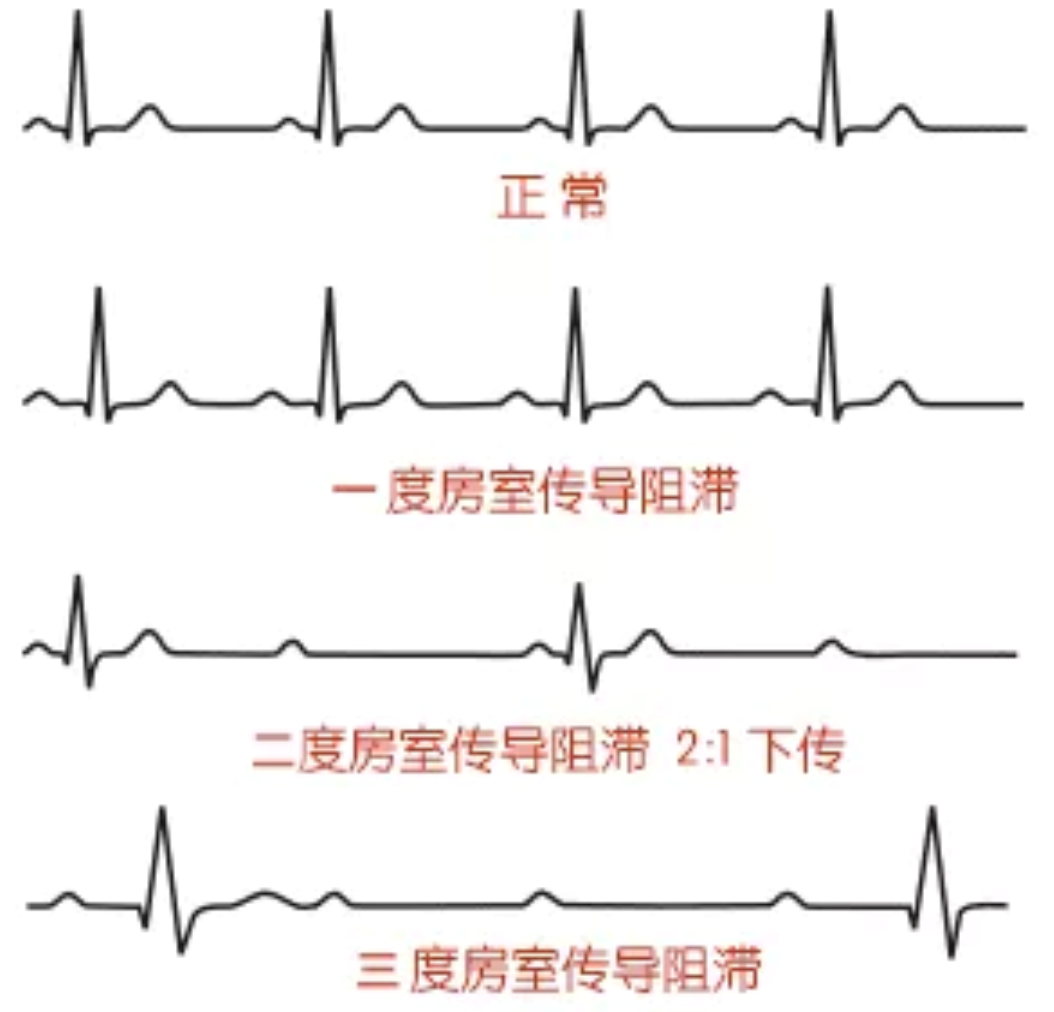
①每个P波后,均有QRS波群;
②PR间期>0.20秒。
(一度房室阻滞;图源:《实用临床心电图手册》)
02 二度房室阻滞部分心房激动不能传至心室,一些P波后没有QRS波群,房室传导比例可能是2: 1;3: 2;3: 1;;4: 3等。通常将二度房室阻滞分为I型和Ⅱ型,二度I型房室阻滞又称文氏现象,或称莫氏I型;二度II型房室阻滞又称莫氏Ⅱ型。
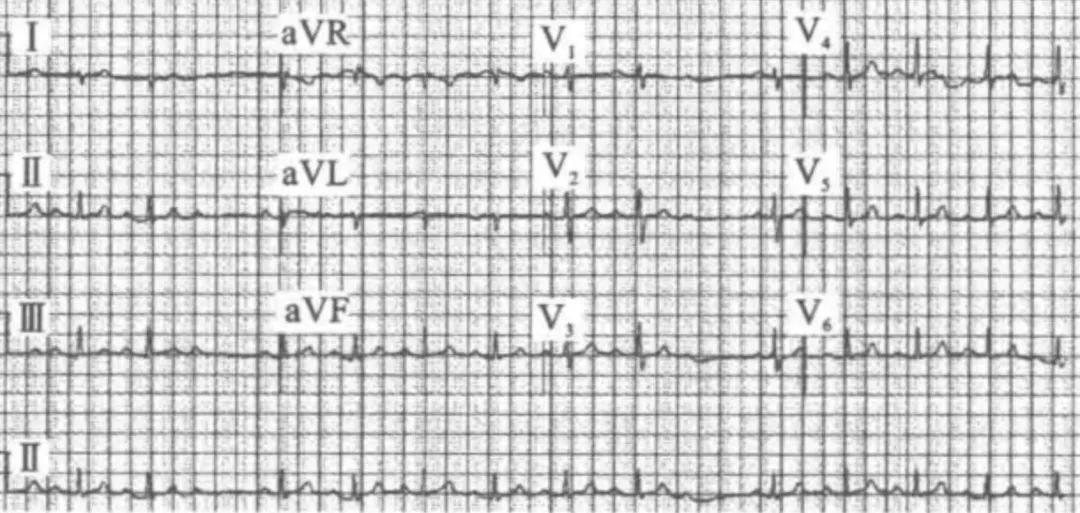
(1)二度I型房室阻滞-文氏现象:是最常见的房室阻滞类型,心房冲动的传导逐渐受阻。表现为:
①PR间期进行性延长,直至P波受阻不能下传至心室;
②RR间期进行性缩短,直至P波不能下传心室;
③包含受阻P波的RR间期<2PP间期。
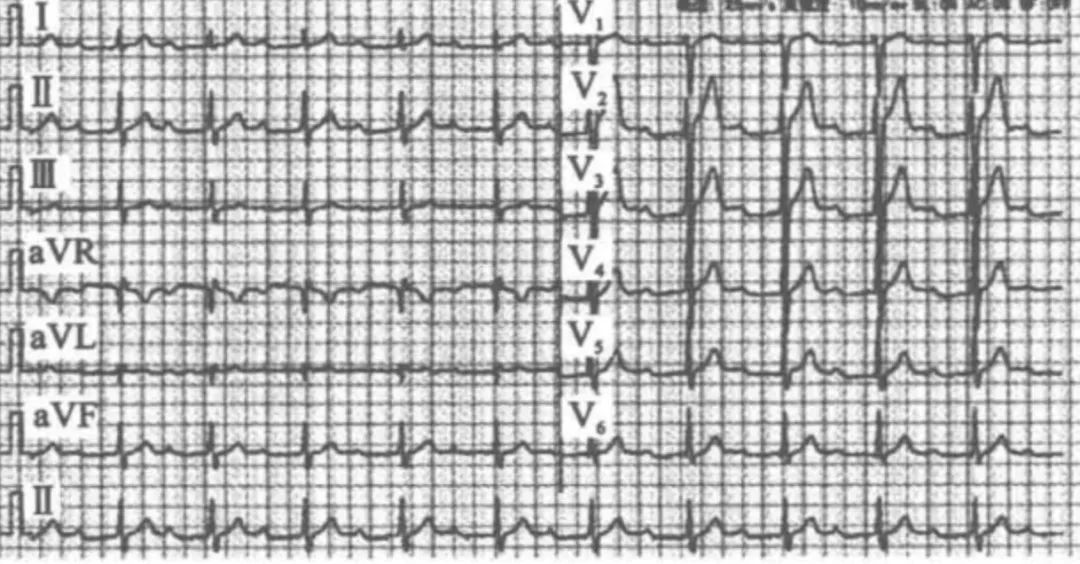
(二度I型房室阻滞;图源:《实用临床心电图手册》)
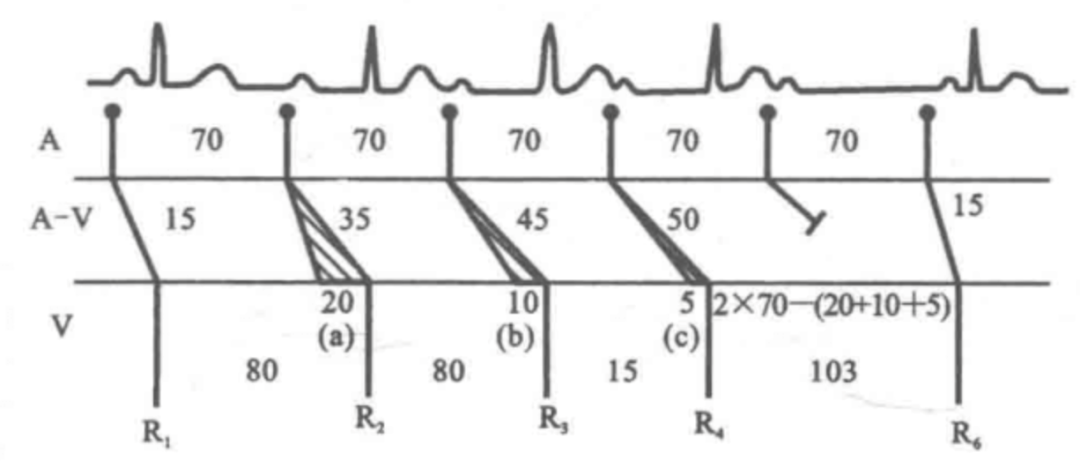
(二度I型房室阻滞示意图:文氏现象开始,PR间期150 ms以后逐渐延长,由350 ms延长至500ms,之后QRS漏搏,结束一次文氏现象。PR间期逐渐延长,但递增量减少(分别为200 ms、100 ms及50 ms);图源:PubMed)
(2)二度II型房室阻滞-莫氏Ⅱ型:心房冲动的传导突然受阻。表现为:
①PR间期恒定不变,可正常或延长;②QRS波群有间期性脱漏,阻滞程度可经常变化。
一度和二度I型房室阻滞,阻滞部位多在房室结,其QRS波群形态与时限均正常;二度II型房室阻滞,其阻滞部位多在希氏束以下,此时QRS波群呈束支阻滞图形。
(二度II型房室阻滞;图源:《实用临床心电图手册》)
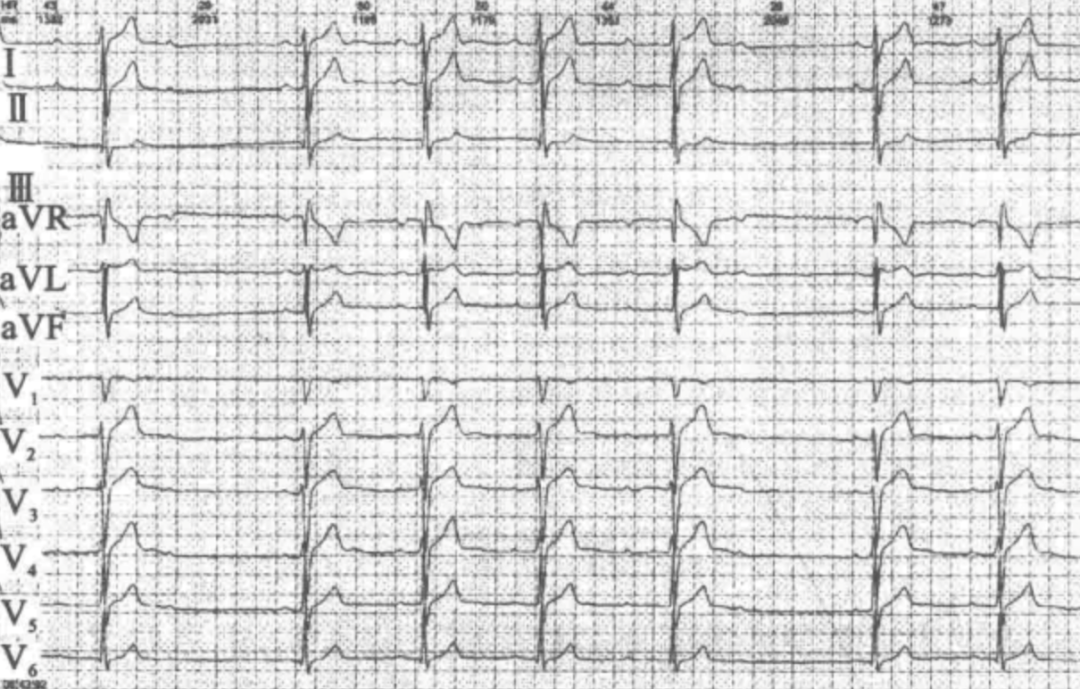
03 三度房室阻滞心房冲动全部不能下传至心室。表现为:
①房室分离;
②心房节律可为窦性或起源于异位,心房率快于心室率;
③心室节律由交界区或心室自主起搏点维持,心室率一般<45次/min;
④RR间期> 2PP间期。另外,心房率一般不宜超过135次/min,因心房率> 135次/min时,不.能除外生理不应期引起的干扰性分离。心房颤动时心室率< 45次/min且室律匀齐也应考虑三度房室阻滞。

(心房扑动、交界性逸搏心律,三度房室阻滞;图源:《实用临床心电图手册》)
QRS波群的形态主要取决于阻滞的部位,如阻滞位于希氏束分支以上,QRS波群不增宽。如阻滞位于双束支,QRS波群增宽或畸形。
三、治疗方案和原则
01 首先针对病因进行,如用抗生素治疗急性感染,肾上腺皮质激素抑制非特异性炎症,阿托品等解除迷走神经的作用。停止应用导致房室阻滞的药物,如用氯化钾静脉滴注治疗低血钾等。
02 药物治疗阿托品(0.5~2.0 mg,静脉注射)适用于阻滞位于房室结的患者。异丙肾上腺素(1~4 μg/min,静脉滴注)适用于任何部位的房室阻滞,但急性心肌梗死患者慎用。药物治疗适用于无心脏起搏条件的应急情况,条件许可时应及早给子临时性或永久性心脏起搏器治疗。
03 起搏治疗房室阻滞的起搏器置入原则几乎与病窦完全一样,即症状性房室阻滞。包括症状性一度、二度和三度房室阻滞。
04 不同程度和类型的房室阻滞的具体治疗方案和原则安装 永久性起搏器前必须排除由其他可逆性因素导致的心律失常。可逆性因素包括:电解质紊乱、长期服用减慢心率药物、下壁心肌梗死所致的缓慢性心律失常、心肌炎、糖尿病、甲状腺功能异常、代谢综合征等。当这些可逆性因素去除后,房室阻滞往往可以消失。
(1)一度房室阻滞:急性一度房室阻滞多是由于心脏的病变或药物中毒所致,需针对病因治疗,较快地控制病情的发展;慢性一度房室阻滞常不需要治疗,但应注意避免使用加重传导延迟的药物。另外,一度房室阻滞是否需要治疗取决于PR间期延长的程度和对心功能的影响。PR<0.35秒,一般对心功能无明显影响,不需要特殊处理。当PR间期持续过度延长(> 0.35秒)时,可引起二尖瓣反流及心功能不全。这时需要给以治疗,可置入双腔起搏器,通过程控AV间期,使二尖瓣反流减少或消失,改善心功能。
(2)二度房室阻滞:I型房室阻滞的阻滞部位多位于房室结,常是良性的,预后较好,无需特殊治疗; Il 型房室阻滞的阻滞部位几乎均位于希-浦系内,易发展成三度房室阻滞,常需要起搏治疗。
任何阻滞部位和类型的二度房室阻滞产生的症状性心动过缓为起搏器置入I类适应证。无症状的二度II 型房室阻滞,心电图表现为宽QRS波群。应列为起搏器置人I类适应证。无症状的二度II型房室阻滞,心电图表现为窄QRS波群,为起搏器置入Ila类适应证。无症状的二度I型房室阻滞,因其他原因行电生理检查中发现阻滞在希氏束内或以下水平,为起搏器置入lla类适应证。
无症状的二度I型房室阻滞,发生于希氏束以上以及未能确定阻滞部位是在希氏束内或以下,应列为起搏器置入II类适应证。
(3)三度房室阻滞:心室率在40次/min以上,无症状者,可不必治疗,如心室率过缓可试给麻黄碱、阿托品、小剂量异丙肾上腺素5~10 mg,每天4次,舌下含化。如症状明显或发生过心源性晕厥,可静脉滴注异丙肾上腺素(1~4 μg/min),并准备安置人工心脏起搏器。
任何阻滞部位的三度房室阻滞伴有下列情况之一者:
①有房室阻滞所致的症状性心动过缓(包括心力衰竭);
②需要药物治疗其他心律失常或其他疾病,而所用药物又能导致症状性心动过缓;
③虽无临床症状,但业已证明心室停搏>3秒或清醒状态时逸搏心率<40次/min;
④射频消融房室交界区导致的三度房室阻滞;
⑤心脏外科手术后发生的不可逆性房室阻滞;
⑥神经肌源性疾病伴发的房室阻滞。无论是否有症状均列为起搏器置入I类适应征,因为传导阻滞随时会加重。
任何部位无症状的三度房室阻滞,清醒时平均心率≥40次/min,尤其是伴有心肌病和左心功能不良,应列为起搏器置入Ila类适应证。
三度房室阻滞患者在紧急情况下,需要安临时心脏起搏器进行抢救,稳定后再安装永久心脏起搏器。当某些病因去除后心律可以恢复正常时,例如急性心肌梗死后或停用地高辛后,也可以只安装临时心脏起搏器。预期可以恢复且不再复发的房室阻滞为起搏器置入III 类适应证。
参考文献
[1]Cao Miaomiao,Chen Li,Sun Chaofeng,Li Guoliang. Transient complete atrioventricular block and ST-segment elevation induced by coronary vasospasm due to iatrogenic hyperkalemia: a case report[J]. Journal of Medical Case Reports,2021,15(1).
[2]刘敏,谢波,刘福强,张俊,秦方.PR间期过度延长伴二度Ⅰ型房室传导阻滞1例[J].心电与循环,2021,40(01):86-87+90.
[3]王淑珍,邓晓奇,熊峰,赵若寒,徐敏,谭焜月,刘春霞,张丽娟.左束支起搏患者心脏机械同步性的早期评估[J].中国循环杂志,2021,36(01):28-33.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#房室阻滞#
93
很全面,学习了
75
#拦路虎#
119
学习了,非常感谢
99
学习了
105
学习
92