European Radiology:MR指纹技术在轻度创伤性脑损伤中的应用
2021-12-28 MedSci原创 MedSci原创
轻度创伤性脑损伤(mTBI)是一个主要公共卫生问题,全世界每年的发病率约为5500万 。虽然大多数患者可完全康复,但仍有一部分患者会出现持续的身体、精神、情绪或认知障碍。

轻度创伤性脑损伤(mTBI)是一个主要公共卫生问题,全世界每年的发病率约为5500万 。虽然大多数患者可完全康复,但仍有一部分患者会出现持续的身体、精神、情绪或认知障碍。
弥漫性轴索损伤被认为是大多数TBI相关损害的主要病理过程。离子失衡导致轴突曲张和其他轴突束的微结构损伤,这一点通常用弥散张量成像(DTI)来评估。然而,DTI结果在解剖位置、改变的性质以及与临床结果的相关性方面有很大的差异。水的局部分子环境的变化可以通过定量评估其纵向(T1)和横向(T2)弛豫时间来检测,但尽管TBI在动物模型中取得了较好的结果,但在人体中的相关研究号相对匮乏。由于大多数弛豫测量法需要较长的采集时间,且只限于单一属性(T1或T2),这阻碍了研究的进一步深入。幸运的是,磁共振指纹打印技术(MRF)能从单一的MRI采集中快速重建不同的参数,因此使定量弛豫测量法的临床应用成为可能。
近日,发表在European Radiology杂志的一项研究评估了基于MRF的弛豫特性(T1、T2)是否与患者的预后有关联,并将结果与已建立的DTI指标分数各向异性(FA)和表观扩散系数(ADC)进行比较,为该类患者的早期诊断及治疗评估提供了技术支持。
对伤后24±10天(时间点1)和伤后90±17天(时间点2)的患者进行临床成像、MRF和DTI采集,并对对照组进行一次图像采集。通过全脑功能、症状描述和神经心理学测试来评估患者的预后。用Mann-Whitney测试比较了12个灰质和白质区域的DTI的ADC和分数各向异性(FA)以及MRF的T1和T2。用Spearman相关性和逻辑回归法评估MR测量和结果之间的双变量关系。
分析了22名患者(38±12岁;17名女性)和18名对照组(32±8岁;12名女性)的数据。14名患者(37±12岁;11名女性)返回了时间点2,而两名患者只提供了时间点2的临床结果数据。在时间点1,患者和对照组在T1、T2和ADC方面没有差异,而MTBI额叶白质的FA则较低。与T2(n = 3)、FA(n = 7)和ADC(n = 2)相比,时间点1的T1和T1的变化与时间点2的临床结果表现出更显著(n = 18)的中度至强的相关性(|r|= 0.6-0.85)。在时间点1的高T1和连续增加的T1中,有5个MR指标对识别时间点2的未康复患者具有最高诊断效能(AUC>0.80)。
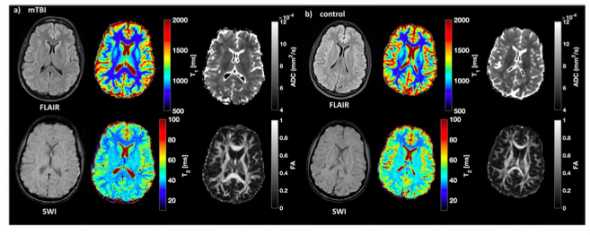
图 创伤性骨折病人和匹配对照组的定性和定量图像示例。34岁女性患者(a)在时间点1的FLAIR和SWI以及T1、T2、ADC和FA图,以及30岁女性(b)的对照图像。注意灰质和白质之间明显的T1和T2差异。
基于MRF的弛豫测量法能够在临床扫描的时间范围内收集水的弛豫时间,在创伤后1个月和3个月时,患者和对照组之间的T1和T2没有明显的差异。然而,1个月的WM T1和1至3个月的WM T1的变化与受伤后3个月的临床和神经认知障碍有关。这些相关性比T2的相关性更强,比DTI的FA和ADC的相关性更强,表明MRF能在定性MRI和DTI之外提供不同程度的预后价值。
原文出处:
Teresa Gerhalter,Martijn Cloos,Anna M Chen,et al.T1and T2quantification using magnetic resonance fingerprinting in mild traumatic brain injury.DOI:10.1007/s00330-021-08235-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
63
#指纹#
71
#创伤性#
99
#创伤#
95
#损伤#
68