Acta Clin Croat:彩色多普勒超声检测早期甲状腺功能亢进视神经病变的眼眶血管的血流变化
2018-11-25 MedSci MedSci原创
克罗地亚斯普利特大学医院中心眼科的LesinM等人近日在Acta Clin Croat上发表了一项重要工作。甲状腺相关眼眶病(TAO)是一种格雷夫斯病的常见表现。在TAO中约有6%的患者会发展为甲状腺功能亢进性视神经病变(DON),而这是TAO最严重的并发症。该研究的目的就是研究其发生过程。
克罗地亚斯普利特大学医院中心眼科的LesinM等人近日在Acta Clin Croat上发表了一项重要工作。甲状腺相关眼眶病(TAO)是一种格雷夫斯病的常见表现。在TAO中约有6%的患者会发展为甲状腺功能亢进性视神经病变(DON),而这是TAO最严重的并发症。该研究的目的就是研究其发生过程。
由于DON可导致永久性损伤,因此在视力损伤的初始阶段,及视力有可能恢复的情况下,及早发现DON是至关重要的。彩色多普勒超声是一种非侵入性诊断方法,可用于早期发现DON。

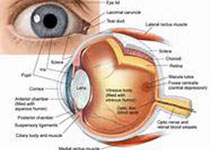
在确诊的36名格雷夫斯病和活动性TAO的患者,其中21名(58%)患有早期DON(eDON),另外15名(42%)没有任何的eDON症状。所有纳入研究的患者均进行了多普勒超声检查以确定颈内动脉、眼动脉和视网膜中央动脉的血流速率等情况。
研究结果显示,彩色多普勒超声检查可以检测到eDON患者的眼眶血流变化。早期发现DON可以进行早期治疗,并可以预防永久性视神经损伤。
原文出处:
Lesin, M., et al., Flow Changes in Orbital Vessels Detected with Color Doppler Ultrasound in Patients with Early Dysthyroid Optic Neuropathy. Acta Clin Croat, 2018. 57(2): p. 301-306.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#甲状腺功能亢进视神经病变#
84
#视神经病变#
0
#血流变化#
59
#多普勒超声#
58
#CRO#
88
#彩色多普勒超声#
59
#OAT#
56
#视神经#
0
#CTA#
44
#甲状腺功能亢进#
116