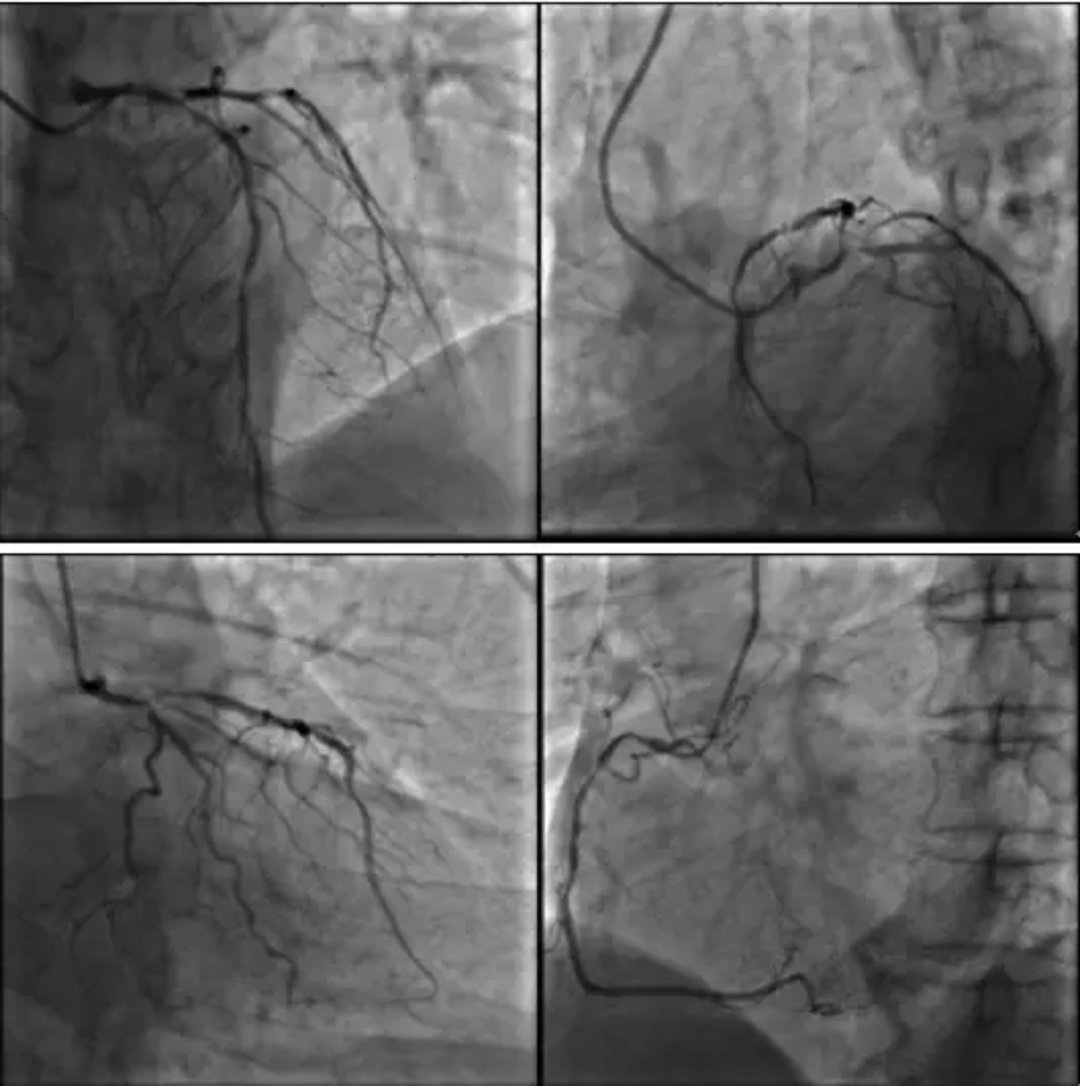
北大人民医院ECMO应用经验:辅助循环“烟囱技术”可减少并发症
2019-05-15 不详 中国循环杂志
北京大学人民医院廉波等研究提示,与直接插管相比,VA-ECMO辅助循环“ 烟囱技术”可改善ECMO 的插管部位出血和远端肢体缺血情况。本组行VA-ECMO 辅助的难治性心力衰竭(心衰)患者37例,均使用同侧股动静脉插管建立ECMO 通路。21例患者接受股动脉切开直接插管,根据远端肢体缺血情况,在ECMO 循环管路上使用ARROW 双腔深静脉插管建立向远端肢体的侧支循环,16例患者接受了“烟囱技术”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#北大人民医院#
68
#并发#
62
#CMO#
59
#人民医院#
78