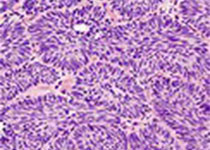
Sci Rep:在前列腺癌细胞中,突变等位基因的定量研究阐释了TP53促使去势抵抗性的遗传基础
2018-09-02 AlexYang MedSci原创
关于人类癌症的本质是遗传疾病,并通过基因变异引起的观点已经有了很详细的阐释,然而在癌症基因的功能研究中,上述观点还没有进行过很好的探索。最近,有研究人员在一个异源群体中,描述了一个简单的基于遗传的方法来快速和灵敏的阐释感兴趣的基因的变异对其宿主细胞的命运的影响,从而监控与致瘤相关的遗传选择。研究人员利用他们的方法,发现了TP53功能的缺失能够通过瞬间增强不依赖雄激素细胞的生长和促使基因组不稳定性的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抗性#
57
#癌细胞#
59
#p53#
66
#TP53#
68
#等位基因#
60
#前列腺癌细胞#
49
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦
79
又是tp53
97
认真学习,不断进步,把经验分享给同好。点赞了!
91