Nat Commun:器官芯片成功模拟月经周期,或有助未来药物研发
2017-03-29 佚名 Nature自然科研
《自然-通讯》发表的论文A microfluidic culture model of the human reproductive tract and 28-day menstrual cycle报告称,使用器官芯片(organ-on-a-chip)技术可以模拟人类生殖系统的28天月经周期。该研究首次表明,不同的生殖系统组织可以和其它组织一起顺利培养一个月,并会释放激素,如同在正常的月经周期中观
《自然-通讯》发表的论文A microfluidic culture model of the human reproductive tract and 28-day menstrual cycle报告称,使用器官芯片(organ-on-a-chip)技术可以模拟人类生殖系统的28天月经周期。该研究首次表明,不同的生殖系统组织可以和其它组织一起顺利培养一个月,并会释放激素,如同在正常的月经周期中观察到的一样。该技术或许能药物发现提供一个平台。
Alex Fan
日益发达的精密加工技术使对材料进行微观尺度的加工成为可能,微流控芯片应运而生。这类装置专门应对微小液量,利用液体自身的表面张力等流体力学特性,通过在材料上加工出刻线、管道、微型阀门等,让液体按规划进行运动和反应。微流控芯片已用于化学、生命科学甚至软体机械控制等方面的研究。在生物医学研究的应用之一即是用人体细胞制备器官芯片,对人体的器官系统进行模拟。目前已有心脏芯片、肺芯片、肾芯片等类型。
本研究就是用器官芯片技术来模拟女性生殖系统的。女性生殖系统由卵巢、输卵管、子宫和子宫颈等不同类型的器官和组织构成,各种激素和组织之间复杂的作用使得在实验室模拟这一系统非常困难。
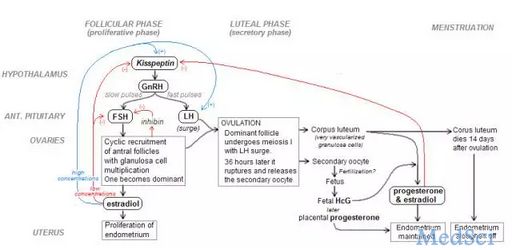
月经周期内各种器官和激素之间的作用。
美国西北大学的Teresa Woodruff及同事制造了单个、两个和五个芯片的微流控平台。在这个五联平台中,作者将小鼠卵巢和人类输卵管、子宫内膜、子宫颈和肝组织结合在一起,在该装置中培养了28天(加入肝组织是为了检验对非生殖系统细胞的作用),持续时间超出此前可达到的水平。在这个装置中,流体能够在组织上流动。通过外加压头,研究者让组织承受一定压力,以驱动液体在组织之间流动,并模仿身体内发生的情况。
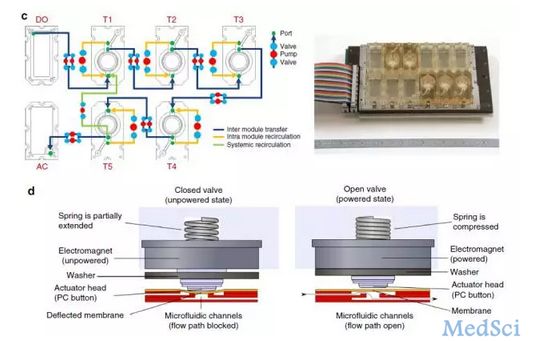
本研究所述包含5种不同组织的五联微流控平台。 Xiao et al.
为了模拟脑垂体激素的影响,作者开发了一套计算激素输入浓度的算法,依此随着时间流逝向系统中输入相应浓度的促卵泡激素(FSH)和人绒毛膜促性腺激素(hCG,和脑垂体分泌的黄体生成素(LH)相仿),以模拟卵泡期生殖系统受到的其他激素影响。最后培养时观察到类似卵泡的结构在卵巢芯片中正常出现,卵泡期后期出现雌激素峰值,孕酮受抑,如同在月经周期中所见的一样。
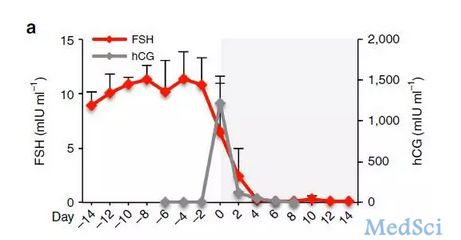
五联微流控平台培养过程中,输入的促卵泡激素(FSH,红)和人绒毛膜促性腺激素(hCG,灰)水平。 Xiao et al.
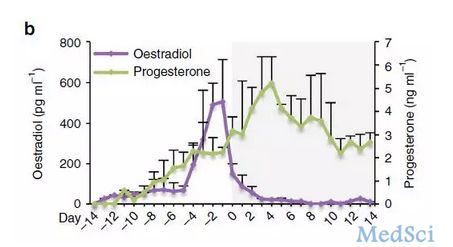
同一系统中雌二醇(紫)和孕酮(绿)水平发生的相应变化。 Xiao et al.
目前该研究存在的缺陷是,它只模拟了激素分泌,而没有反映生殖系统的全部功能(养育胎儿),也没有表明免疫系统等其它因素可能存在的影响。但是,这标志着人们对于理解生殖系统功能迈出了重要一步,有望为未来的药物发现(避孕或不孕症治疗)或毒理研究铺平道路。
对于生物医学来说,器官芯片的一大好处在于可以更准确地模拟实际的人体环境,从而提高药物研发的效率。有句话说得好,“人不是70公斤重的老鼠”。动物模型的一大局限性是它们并非人类,所以实验室内的动物实验有时可能无法反应药物在人体内的真实效应。而用人类细胞制备的器官芯片进行研究则可能有效克服这一局限性,在实验室阶段便直接以具有功能的人类组织为对象进行药物研发。
原始出处:
Shuo Xiao, Jonathan R. Coppeta, Hunter B. Rogers, et al.A microfluidic culture model of the human reproductive tract and 28-day menstrual cycle.Nature Communications.28 March 2017.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
69
#COMMUN#
51
#器官芯片#
61
#研发#
76
#药物研发#
54
#月经#
66
#芯片#
55
类器官未来大有用途
72
看看了解一下
65
签到学习了很多。
82