窦性心律:齐或不齐安全吗?
2015-07-24 YoungTsau 医学界心血管微信
作者:YoungTsau,医学博士,中山大学医学院毕业,美国耶鲁大学博士 正常心脏活动依靠窦房结发出的周期性电脉冲,控制心房和心室有规律的收缩,将血液供应至全身。心脏的电脉冲起源、周期性、节律性、传导时程、传导路径等任何异常,都可能会引起心脏血液动力学变化,影响全身血液供应,严重时可导致生命危险。 通常医生说到窦性心律,都认为是安全的,而对于窦性心律不齐的解读却是语焉不详。事实上,即使是起
作者:YoungTsau,医学博士,中山大学医学院毕业,美国耶鲁大学博士
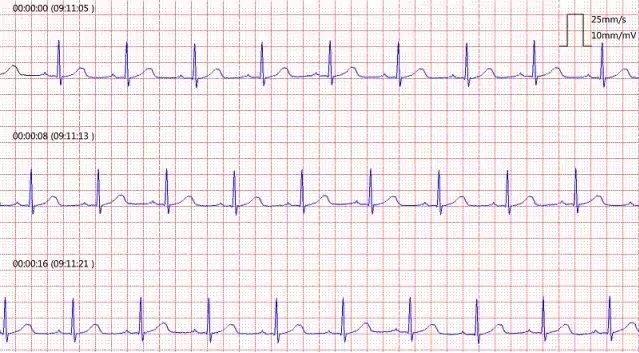
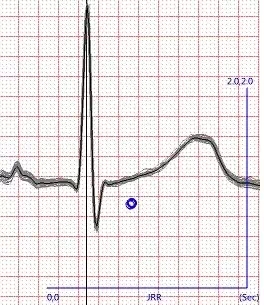
通常医生说到窦性心律,都认为是安全的,而对于窦性心律不齐的解读却是语焉不详。事实上,即使是起源于窦房结的窦性心律,虽然暂时没有生命安全问题,也可能意味着心脏意外的风险。窦性心律不齐的现象非常普遍,那么,不同的窦性心律不齐是怎样产生的?又如何快速判断?
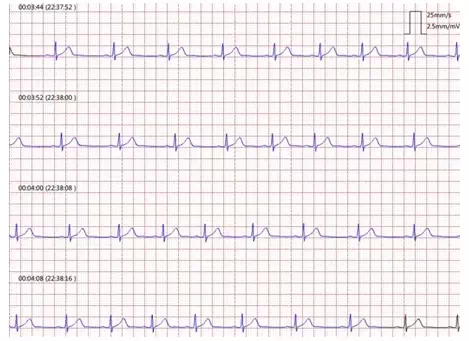
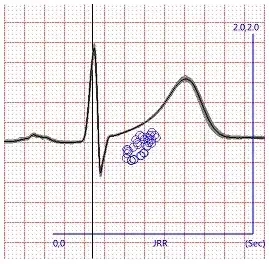
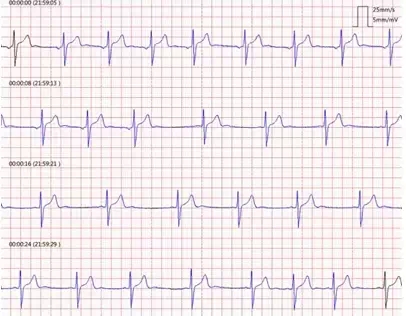
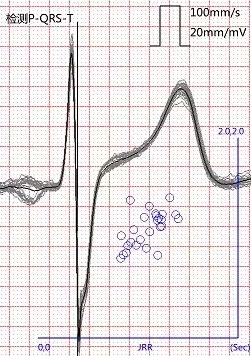
窦性心律不齐可分为正常生理性和病理性两种,后者有潜在心脏意外风险。生理性的窦性心律不齐与呼吸引起的植物神经的张力放电频率变化有关,常见于青少年和经常运动锻炼者。心电检查表现为心动周期逐渐改变时间长度,好像潮汐那样,并且改变可与呼吸相关。下图为一例运动员的心电检查:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了...
212
期待有更多研究
184
受用
222
#窦性心律#
108
区别对待
140
涨知识了
192