Nat Cell Biol:参与免疫反应的蛋白,也在促进癌症发展
2019-12-03 佚名 中国生物技术网
发表在《Nature Cell Biology》上的一篇新研究中,来自美国德克萨斯大学MD安德森癌症中心的研究团队发现,一种参与微生物免疫反应的蛋白质也可以促进癌症的发展,并抑制对疾病的免疫反应。
该研究团队在肺癌小鼠模型中发现,当TANK结合激酶1 (TBK1)及其衔接子TBK结合蛋白1 (TBKBP1)在被生长因子而不是先天免疫机制激活时,有助于肿瘤的发生。
研究通讯作者、免疫学教授Suno-Cong Sun博士说:“我们的研究也是第一次提供了TBK1在癌细胞中介导免疫抑制的证据,表明靶向TBK1将抑制肿瘤生长并促进抗肿瘤免疫。”
最近的研究表明,通常介导对病毒或细菌产生1型干扰素诱导作用的TBK1,还可以促进KRAS依赖性癌细胞的生存与繁殖。为此,Sun团队开始确定TBK1对癌细胞的影响及其在体内癌症发展中的作用。
在后续一系列的实验中,研究人员发现TBK1和TBKBP1形成一个生长因子信号转导轴,并激活mTORC1,以促进肿瘤的发展。该途径包括TBKBP1通过称为CARD10的支架蛋白将TBK1募集到蛋白激酶C-theta(PKCθ),从而使PKCθ激活TBK1。
为了测试这种蛋白质的治疗潜力,他们用免疫调节剂Amlexanox来治疗KRAS诱发的肺癌小鼠。Amlexanox是美国食品和药物管理局(FDA)批准用于治疗某些口腔溃疡的药物。该药物最近被鉴定为TBK1抑制剂。注射Amlexanox小鼠的肺肿瘤数量和体积急剧减少。
KRAS驱动的癌症对免疫反应有抵抗力,但研究人员发现,Amlexanox对肿瘤敏感,阻断了免疫T细胞上的CTLA-4检查点。
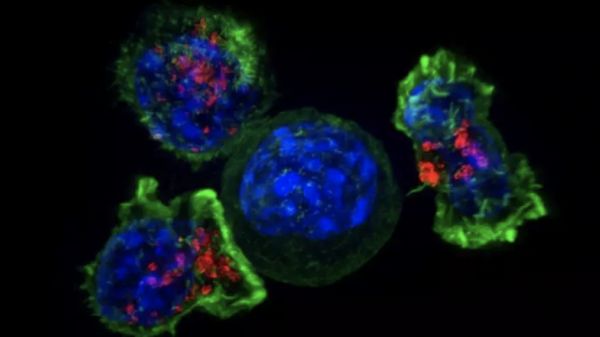
在KRAS驱动的小鼠模型中敲除TBK1增加了CD4辅助T细胞和CD8杀伤T细胞在小鼠肺部的频率。在另一只小鼠模型中进行的类似实验也降低了免疫抑制的髓样抑制细胞的频率。
其他实验表明,TBK1可以促进糖酵解(一种也抑制免疫系统的糖燃烧代谢过程),以及PD-L1的增加。PD-L1是肿瘤细胞上的一种蛋白质,通过与细胞表面的PD-1蛋白连接来关闭对T细胞的攻击。
Amlexanox和抗CTLA-4免疫治疗可以刺激免疫反应,并在小鼠模型中减少肿瘤的体积和频率。
Sun说:“我们将继续使用动物模型研究TBK1在不同类型免疫细胞中的信号传导功能,并使用临床前癌症模型评估TBK1的治疗潜力。”
虽然Amlexanox已经在治疗2型糖尿病和肥胖症的临床试验中进行了测试,但目前还没有开放的临床试验来测试该药物对癌症的疗效。Sun表示,他的团队将继续进行必要的临床前研究,以为临床试验奠定基础,包括确定Amlexanox是否可能对其他类型的癌症有效。
Lele Zhu, Yanchuan Li, Xiaoping Xie,et al.TBKBP1 and TBK1 form a growth factor signalling axis mediating immunosuppression and tumourigenesis.Published: 02 December 2019.Nature Cell Biology (2019).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biol#
69
#Nat#
50
#Bio#
55
#CEL#
74
#Cell#
63
#免疫反应#
77
研究新颖,受益良多
117
研究新颖,受益良多
131
研究新颖,受益良多
153
研究新颖,受益良多
136