JAMA Oncol:DDGP方案 vs SMILE方案治疗新诊断的局部晚期结外自然杀伤/T细胞淋巴瘤
2022-06-23 MedSci原创 MedSci原创
对于新诊断的局部晚期ENKL患者,DDGP方案显示出了良好的初步疗效
结外自然杀伤/T细胞淋巴瘤 (ENKL) 是成熟T细胞和NK细胞淋巴瘤的一种亚型,以EB病毒感染为特征。临床上,ENKL病变常侵犯鼻腔、鼻咽、鼻窦等中线结构。部分ENKL甚至可能发展为噬血细胞综合征,导致预后不良。
基于左旋天冬酰胺酶的SMILE(地塞米松、甲氨蝶呤、异环磷酰胺、左旋天冬酰胺酶和依托泊苷)化疗方案在ENKL患者中展现出了比含蒽环类药物方案更高的有效率和生存率。但是,该方案的安全性尚差强人意。目前还缺乏一种耐受性良好、疗效佳的治疗方案。
该研究是一项在我国开展的开放标签、多中心的随机临床试验,旨在评估DDGP(地塞米松、顺铂、吉西他滨和培门冬酶)方案与SMILE方案在新确诊的晚期(III/IV期)ENKL患者中的疗效和安全性。
14-70岁的ECOG表现状态0-2分的新确诊的III/IV期ENKL患者被随机分至DDGP组或SMIE组,各组患者都接受了6个疗程的治疗(21天/疗程)。主要终点是无进展生存期(PFS),次要终点包括总缓解率和总生存率(OS)。
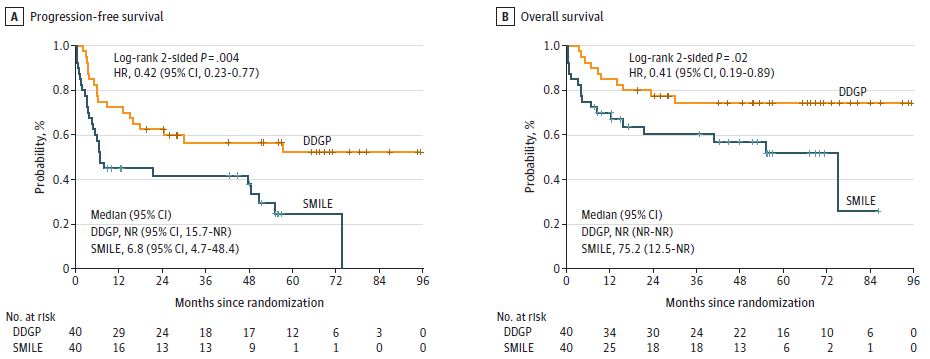
两组的无进展生存率和总生存率
共87位患者被随机分组,其中80位接受了研究治疗(两组各40位);中位年龄43岁,51位(64%)男性。两组患者的基线特征相近。中位随访了41.5个月后,DDGP组和SMILE组的中位PFS分别是未达到和6.8个月(HR 0.42, p=0.004),中位OS分别是未达到和75.2个月(HR 0.41, p=0.02)。DDGP组的3年PFS率和5年OS率均明显高于SMILE组(3年PFS率:56.6% vs 41.8%;5年OS率:74.3% vs 51.7%)。DDGP组的总缓解率明显高于SMILE组(90.0% vs 60.0%,p=0.002)。
两组的治疗反应
3/4级血液毒性反应更常见于SMILE组(SMILE组 vs DDGP组:白细胞减少症,85.0% vs 62.5%,中性粒细胞减少症,85.0% vs 65.0%)。
综上,该研究结果显示,对于新诊断的局部晚期ENKL患者,DDGP方案显示出了良好的初步疗效。
原始出处:
Wang X, Zhang L, Liu X, et al. Efficacy and Safety of a Pegasparaginase-Based Chemotherapy Regimen vs an L-asparaginase–Based Chemotherapy Regimen for Newly Diagnosed Advanced Extranodal Natural Killer/T-Cell Lymphoma: A Randomized Clinical Trial. JAMA Oncol. Published online June 16, 2022. doi:10.1001/jamaoncol.2022.1968.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新诊断#
77
#局部晚期#
65
#Oncol#
67
#细胞淋巴瘤#
68
#T细胞淋巴瘤#
96
#局部#
76
JAMA上文章都是顶级的,谢谢梅斯及时上新
56