NEJM:常年咀嚼烟叶导致口腔鳞状细胞癌的发生
2017-09-22 MedSci MedSci原创
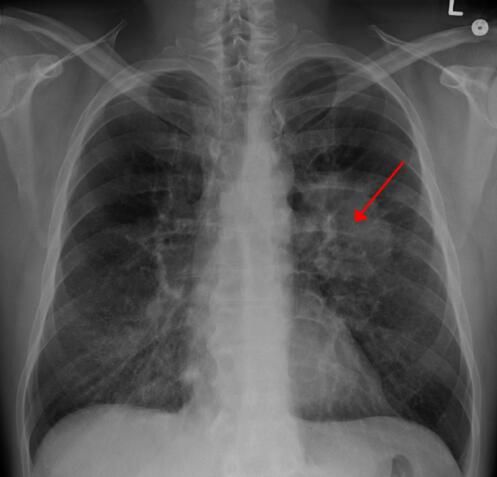
患者,女,54岁,因口腔肿胀疼痛一年就诊于口腔诊所。 患者有经常咀嚼散烟叶的习惯,将烟叶放在颌骨和舌之间,每天多达五次,长达十多年。口内检查显示下颌左内侧病变区为不规则硬化病变,尺寸最大为3厘米(图A)。组织切片活检显示结缔组织中具有变色、多形性细胞和“角化珠”(图B)的浸润性鳞状细胞癌。计算机断层扫描和正电子发射断层扫描显示没有骨或淋巴结受累。 鳞状细胞癌是口腔最常见的肿瘤类型。患将
患者,女,54岁,因口腔肿胀疼痛一年就诊于口腔诊所。
患者有经常咀嚼散烟叶的习惯,将烟叶放在颌骨和舌之间,每天多达五次,长达十多年。口内检查显示下颌左内侧病变区为不规则硬化病变,尺寸最大为3厘米(图A)。组织切片活检显示结缔组织中具有变色、多形性细胞和“角化珠”(图B)的浸润性鳞状细胞癌。计算机断层扫描和正电子发射断层扫描显示没有骨或淋巴结受累。

鳞状细胞癌是口腔最常见的肿瘤类型。患将癌组织整块切除,并进行节段性下颌切除术,使用血管化游离腓骨瓣进行骨移植及选择性颈清扫术。病理分析显示未累及骨或淋巴结,无肿瘤边缘。
建议病人停止使用烟草制品。治疗两年后,未复发。
原始出处:
Tanay V. Chaubal,Renjeet A. Bapat. Squamous-Cell Carcinoma of the Mouth. N Engl J Med 2017; 377:1188September 21, 2017DOI: 10.1056/NEJMicm1701886.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
59
#咀嚼#
62
#口腔鳞状细胞癌#
74
学习了谢谢分享!!
82
很好的文章.学习了
83