张艳桥教授:(K)RAS突变型晚期结直肠癌的治疗
2017-12-13 佚名 中国医学论坛报
黑龙江省消化道肿瘤诊疗中心主任,博士生导师。CSCO结直肠癌专业委员会副主任委员,中国医师协会外科分会MDT指导委员会,中国抗癌协会肿瘤药物临床研究专业委员会常委,中国抗癌协会肿瘤靶向治疗专业委员会常委,黑龙江省医学会肿瘤靶向治疗专业委员会主任委员。
张艳桥 教授 哈尔滨医科大学附属肿瘤医院
黑龙江省消化道肿瘤诊疗中心主任,博士生导师。CSCO结直肠癌专业委员会副主任委员,中国医师协会外科分会MDT指导委员会,中国抗癌协会肿瘤药物临床研究专业委员会常委,中国抗癌协会肿瘤靶向治疗专业委员会常委,黑龙江省医学会肿瘤靶向治疗专业委员会主任委员。
结直肠癌是世界范围内常见的恶性肿瘤。我国结直肠癌死亡率居肿瘤的第4位。随着我国居民生活水平提高、饮食结构改变和人口老龄化,结直肠癌发病率明显提高,并呈年轻化趋势。
目前,以化疗为主的综合治疗是mCRC的主要治疗方法。近年来,靶向药物的出现为mCRC患者带来更多的临床获益。
此外,如何筛选出靶向药物治疗可能的获益人群,预测靶向药物的疗效,也是mCRC治疗领域中的热点。其中以RAS基因研究最为广泛。
随着基础与临床研究的不断深入,mCRC的治疗模式正在发生转变。
RAS突变与mCRC
人RAS家族由Harvey(H)-,Kirsten(K)-和N-RAS 3种癌基因亚型组成。结直肠癌中,(K)RAS突变率约为40%,(N)RAS突变率约为1%-3%,而尚无有意义的(H)RAS突变报道。
1998年,著名的美国国立癌症研究所杂志(J Natl Cancer Inst)刊登了多国、多中心协作研究。结果显示,(K)RAS突变增加各分期患者的死亡风险,是结直肠癌的不良预后因素。
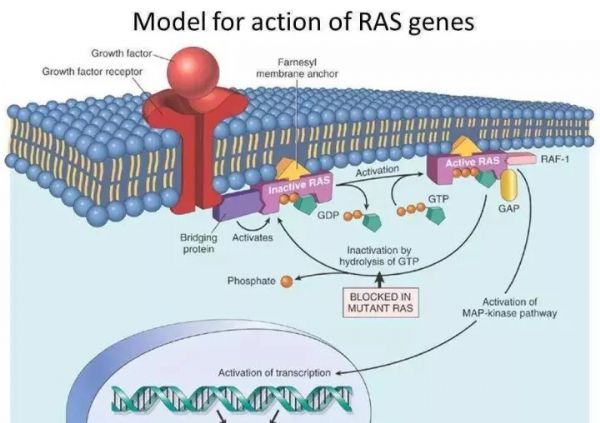
(K)RAS突变能使得RAS-RAF-MAPK信号通路不再依赖EGFR上游信号而持续异常激活。因此,存在(K)RAS基因突变的患者,使用抗EGFR药物治疗不敏感。
(K)RAS基因状态是mCRC抗EGFR治疗的重要预测指标。既往研究表明,(K)RAS突变的mCRC患者不能从化疗联合抗EGFR治疗中获益。
(K)RAS突变还能使(K)RAS基因激活,上调血管内皮生长因子(VEGF)表达量,刺激肿瘤血管生成。VEGF是(K)RAS 突变细胞在体内形成肿瘤的关键调节因子,抑制VEGF能显著抑制突变细胞的致瘤能力,而保留VEGF功能的突变细胞出现快速的侵袭性生长。
贝伐珠单抗是针对VEGF的单克隆抗体,已被美国食品与药物管理局(FDA)批准联合化疗用于mCRC的一线治疗。目前研究认为,mCRC组织中存在VEGF高表达预示较差的预后。在mCRC患者中使用贝伐珠单抗治疗14天后,其血浆平均游离VEGF水平显著降低,是其发挥抗肿瘤作用的主要机制。
基于上述重要的研究结果,美国国家综合癌症网络(NCCN)指南推荐,对于所有结直肠癌患者,在诊断mCRC时需检测(K)RAS基因状态,有助于选择合适的个体化治疗方案。
贝伐珠单抗在(K)RAS突变型患者中的数据回顾
AVF2107g是贝伐珠单抗第1个III期临床研究,基于该研究结果,贝伐珠单抗成为第1个被美国FDA批准的抗肿瘤血管生成药物用于治疗mCRC。
研究结果显示,贝伐珠单抗联合化疗,较单纯化疗,能显著延长患者的无进展生存期(PFS)(10.6个月 vs 6.2个月)和总生存期(OS)(20.3个月 vs 15.6个月)。更为重要的是,无论是(K)RAS 野生型,还是突变型mCRC患者,均能从中获益。
另有Meta分析结果显示,相比单纯化疗,贝伐珠单抗联合化疗在全身治疗中表现出明确生存获益,并且不受(K)RAS基因状态的影响。
真实世界经验
2017年美国临床肿瘤学会-胃肠道肿瘤研讨会(ASCO-GI)上,来自日本的回顾性研究结果显示,在(K)RAS突变mCRC患者中,贝伐珠单抗联合两药化疗优于单纯化疗,中位PFS(13.0个月 vs 8.4个月)和中位OS(32.4个月 vs 27.1个月)均获益。
我国秦叔逵教授牵头进行的1项多中心、前瞻性、非干预队列研究(REACT研究)中,使用贝伐珠单抗联合化疗作为一线或二线治疗方案,(K)RAS 野生型和突变型患者的中位PFS组间无显著差异(9.8个月 vs 8.6个月)。
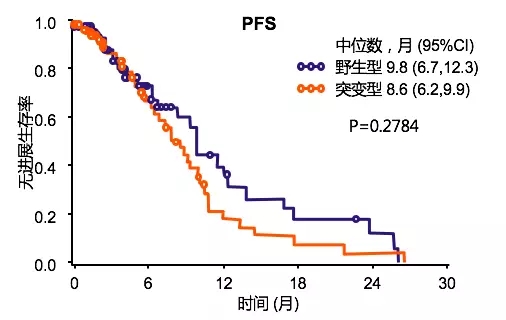
捷克大样本登记研究结果得出相似结论,(K)RAS野生型和突变型患者,一线使用贝伐珠单抗联合化疗,两组中位PFS(11.5个月 vs 11.4个月)和中位OS(30.7个月 vs 28.4个月)均无显著差异。
上述研究结果均表明,(K)RAS基因型不影响一线贝伐珠单抗联合化疗能取得的临床获益。
诊疗指南推荐
2017年NCCN结肠癌指南:推荐贝伐珠单抗联合化疗(包括FOLFOX,CAPEOX,FOLFIRI等)为mCRC的一线治疗方案。
2016年欧洲临床肿瘤内科学会(ESMO)mCRC指南共识:以疾病控制为治疗目标的mCRC患者,包括RAS 野生型或突变型,均推荐贝伐珠单抗联合双药化疗联合为一线全身治疗方案。
2017年中国临床肿瘤学会(CSCO)结直肠癌指南:在RAS突变的mCRC患者中,推荐贝伐珠单抗联合化疗为基本治疗策略。
总结
1. (K)RAS是mCRC中最常见的RAS突变类型。
2. (K)RAS突变能上调VEGF表达,从而促进mCRC肿瘤血管生成。而贝伐珠单抗能有效抑制VEGF活性,延缓肿瘤的生长和转移。
3. 循证学依据已证实,贝伐珠单抗联合化疗能使(K)RAS 野生型/突变型mCRC患者均获益。
4. 诊疗指南推荐贝伐珠单抗联合化疗作为(K)RAS突变型mCRC患者的一线标准治疗。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#晚期结直肠癌#
55
#RAS突变型#
64
#突变型#
48
#结直肠#
56
#RAS突变#
55