JCO:局部晚期HCC患者是否推荐放射性栓塞治疗
2018-03-11 慧语 肿瘤资讯
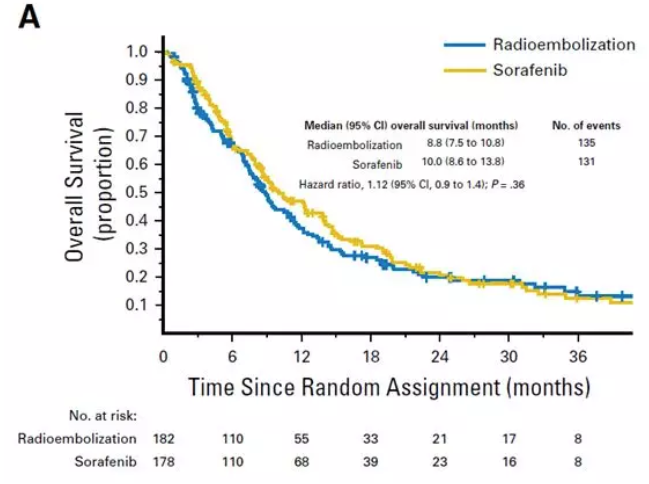
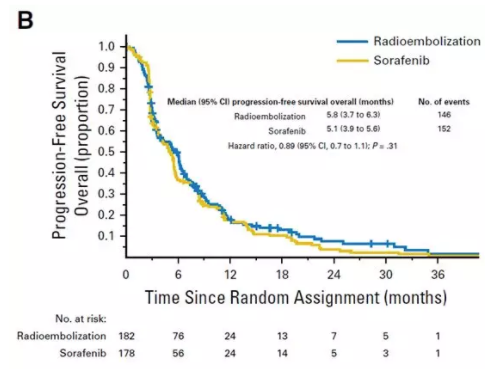
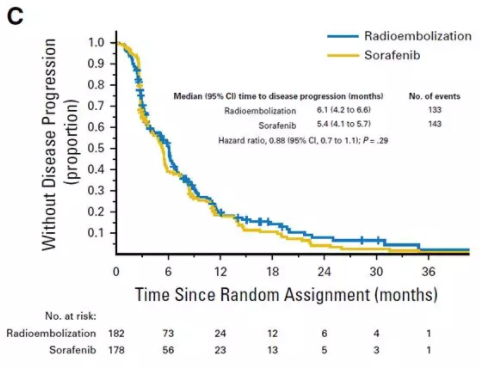
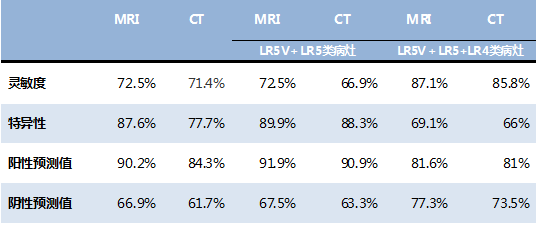
SIRveNIB(选择性体内放射治疗 vs. 索拉菲尼)是一项开放标签、研究者发起的三期临床试验(NCT01135056)。研究对比了Y-90树脂微球与每日800mg索拉菲尼治疗局部晚期不适合手术切除HCC患者的疗效。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#局部晚期#
52
#晚期HCC#
62
#JCO#
52
#HCC#
69
#局部#
56
学习了.涨知识
76
谢谢分享.学习了
78
看看
55
好好学习天天向上
60
学习了
71