Cell:哇!单基因可逆转结肠癌 重建正常组织功能
2015-06-24 佚名 生物谷
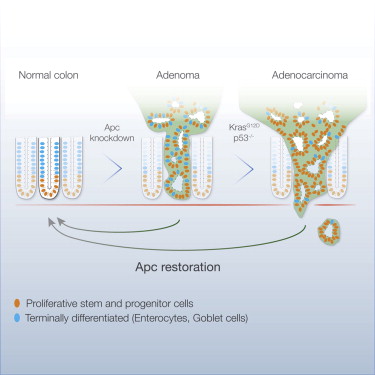
近日,来自美国的科学家在国际学术期刊cell发表了一项最新研究进展,与以往直接杀死肿瘤细胞的策略不同,他们发现在小鼠中将一个与人类结肠癌有关的基因恢复到正常水平可以抑制肿瘤生长并在4天内重建正常的小肠功能。更令人惊奇的是,肿瘤在两周内慢慢消除,癌症症状也在随后的几个月内得到了改善。结肠癌是发达国家中导致癌症相关死亡的第二号杀手,每年全世界大约有700,000人死于结肠癌。目前治疗晚期结肠癌的主要策
近日,来自美国的科学家在国际学术期刊cell发表了一项最新研究进展,与以往直接杀死肿瘤细胞的策略不同,他们发现在小鼠中将一个与人类结肠癌有关的基因恢复到正常水平可以抑制肿瘤生长并在4天内重建正常的小肠功能。更令人惊奇的是,肿瘤在两周内慢慢消除,癌症症状也在随后的几个月内得到了改善。结肠癌是发达国家中导致癌症相关死亡的第二号杀手,每年全世界大约有700,000人死于结肠癌。目前治疗晚期结肠癌的主要策略还是不同化疗药物的联合治疗,这种方法毒性大并且治疗效率并不高,但在过去十年中,结肠癌的治疗仍以此方法为主。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
48
#Cell#
51
可以
93
看看
112
怎么实现呢?
103
基因很强大
150