Sci Transl Med:纳米粒携带抗癌药可有效抵御癌症发展
2012-04-10 T.Shen 生物谷
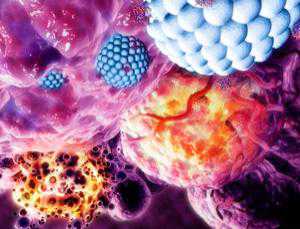
图中显示的是纳米粒携带抗癌药物导致癌细胞破坏崩解;蓝色为纳米粒,紫色为癌细胞(Image: Medi-mation/Science Photo Library) Copyright ®版权归生物谷所有,若未得到Bioon授权,请勿转载。 近日,国际著名杂志Science Translational Medicine在线刊登了国外研究人员最新研究成果“Preclinical Develo

图中显示的是纳米粒携带抗癌药物导致癌细胞破坏崩解;蓝色为纳米粒,紫色为癌细胞(Image: Medi-mation/Science Photo Library)
Copyright ®版权归生物谷所有,若未得到Bioon授权,请勿转载。
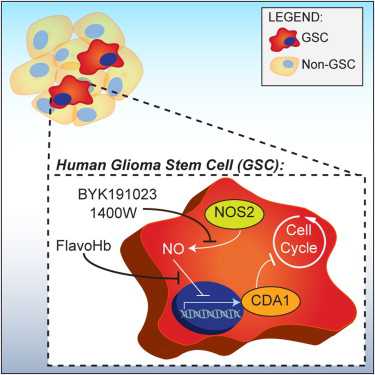
近日,国际著名杂志Science Translational Medicine在线刊登了国外研究人员最新研究成果“Preclinical Development and Clinical Translation of a PSMA-Targeted Docetaxel Nanoparticle with a Differentiated Pharmacological Profile”,文章中研究者揭示了用纳米粒携带抗癌药物对于治疗癌症效果显著。
纳米粒运输治疗法(Drug-smuggling nanoparticles)将会是最新的抵御癌症的方法,早期的实验结果显示,通过纳米粒运输癌症药物治疗的方法可以明显降低人类肿瘤的大小。来自美国波士顿的研究者将癌症药物多西紫杉醇(docetaxel)填入纳米粒中,然后注射入17个癌症患者的血液中,这些患者对药物有一定的耐药性,经过42天后,这些癌症患者中,有两个患者的肿瘤缩小了,其余的患者肿瘤也不再生长了。
当把这种含有癌症药物的纳米粒注射入人的机体内时,多西紫杉醇并不能够识别出健康的细胞核癌细胞,然而,纳米粒却可以起到识别的作用,它可以通过于肿瘤细胞表面的分子反应来识别肿瘤细胞,从而释放抗癌药物,达到抑制肿瘤生长的目的。而且针对每一个肿瘤细胞仅仅需要不到80%的药物。
研究者Jeffrey Hrkach表示,医生们可以自由控制用药浓度,而不需要担心药物的毒性负面效应,不过我们还需要进行更多的临床试验要确定用药量。(生物谷:T.Shen编译)
Copyright ®版权归生物谷所有,若未得到Bioon授权,请勿转载。

doi:10.1126/scitranslmed.3003651
PMC:
PMID:
Preclinical Development and Clinical Translation of a PSMA-Targeted Docetaxel Nanoparticle with a Differentiated Pharmacological Profile
Jeffrey Hrkach1, Daniel Von Hoff2, Mir Mukkaram Ali1, Elizaveta Andrianova1, Jason Auer1, Tarikh Campbell1, David De Witt1, Michael Figa1, Maria Figueiredo1, Allen Horhota1, Susan Low1, Kevin McDonnell1, Erick Peeke1, Beadle Retnarajan1, Abhimanyu Sabnis1, Edward Schnipper1, Jeffrey J. Song1, Young Ho Song1, Jason Summa1, Douglas Tompsett1, Greg Troiano1, Tina Van Geen Hoven1, Jim Wright1, Patricia LoRusso3, Philip W. Kantoff4, Neil H. Bander5, Christopher Sweeney4, Omid C. Farokhzad6,*, Robert Langer7,* and Stephen Zale1,*
We describe the development and clinical translation of a targeted polymeric nanoparticle (TNP) containing the chemotherapeutic docetaxel (DTXL) for the treatment of patients with solid tumors. DTXL-TNP is targeted to prostate-specific membrane antigen, a clinically validated tumor antigen expressed on prostate cancer cells and on the neovasculature of most nonprostate solid tumors. DTXL-TNP was developed from a combinatorial library of more than 100 TNP formulations varying with respect to particle size, targeting ligand density, surface hydrophilicity, drug loading, and drug release properties. Pharmacokinetic and tissue distribution studies in rats showed that the NPs had a blood circulation half-life of about 20 hours and minimal liver accumulation. In tumor-bearing mice, DTXL-TNP exhibited markedly enhanced tumor accumulation at 12 hours and prolonged tumor growth suppression compared to a solvent-based DTXL formulation (sb-DTXL). In tumor-bearing mice, rats, and nonhuman primates, DTXL-TNP displayed pharmacokinetic characteristics consistent with prolonged circulation of NPs in the vascular compartment and controlled release of DTXL, with total DTXL plasma concentrations remaining at least 100-fold higher than sb-DTXL for more than 24 hours. Finally, initial clinical data in patients with advanced solid tumors indicated that DTXL-TNP displays a pharmacological profile differentiated from sb-DTXL, including pharmacokinetics characteristics consistent with preclinical data and cases of tumor shrinkage at doses below the sb-DTXL dose typically used in the clinic.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Transl#
51
#纳米粒#
62
#TRA#
0
#抗癌药#
69
#Med#
0