NEJM:艾滋病患者HPV相关的口腔乳头瘤样增生-病例报道
2016-06-30 MedSci MedSci原创
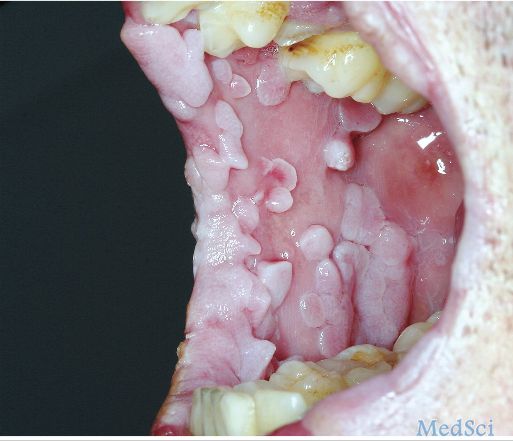
患者男性,36岁,患有获得性免疫缺陷综合征(AIDS)和卡波西肉瘤,2年前口腔内开始出现广泛的无痛性乳头瘤样病变(如下图所示)。患者的性取向为男性,其男朋友存在生殖器疣病史。采用高活性抗逆转录病毒疗法治疗患者。血液中人类免疫缺陷病毒(HIV)1型的水平低于20拷贝/ml,和CD4 + T细胞计数为318个/ml。体格检查显示,患者存在广泛的唇、腭和口腔口腔疣状结节病变与尖锐湿疣表现一致。组织病理学
患者男性,36岁,患有获得性免疫缺陷综合征(AIDS)和卡波西肉瘤,2年前口腔内开始出现广泛的无痛性乳头瘤样病变(如下图所示)。
患者的性取向为男性,其男朋友存在生殖器疣病史。
采用高活性抗逆转录病毒疗法治疗患者。
血液中人类免疫缺陷病毒(HIV)1型的水平低于20拷贝/ml,和CD4 + T细胞计数为318个/ml。体格检查显示,患者存在广泛的唇、腭和口腔口腔疣状结节病变与尖锐湿疣表现一致。组织病理学和免疫组化研究证实为人类乳头状瘤病毒(HPV)6型和11型感染。
在随后的2年中,患者接受多个疗程的二氧化碳激光治疗以消除口腔病变。
与未合并HIV感染的患者相比,合并感染HIV的患者其HPV相关的疣状病变可更持久,更广泛,侵袭性更强。免疫监视(CD4 + T细胞计数低于200个/ml)受损不仅会减少HPV常规治疗的有效性,还会提高尖锐湿疣复发的风险。
原始出处:
Jacobo Limeres Posse, Crispian Scully, Oral HPV-Associated Papillomatosis in AIDS. N Engl J Med 2016; 374:2585June 30, 2016DOI: 10.1056/NEJMicm1512047.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好文章,受益
101
#艾滋病患者#
59
赞了!深度好文,学习。
102
文章不错
118
好恐怖啊
121