JAMA:世卫组织研究证实IL-6抑制剂可降低新冠肺炎住院患者死亡风险
2021-07-13 MedSci原创 MedSci原创
新冠肺炎住院患者使用IL-6抑制剂治疗可降低28天死亡风险。

全身炎症和宿主免疫反应失调引起的过度炎症和IL-6水平升高与新冠肺炎住院患者的不良临床结果相关,但已完成的几个IL-6拮抗剂对新冠肺炎住院患者治疗的试验结论却差异很大,部分研究认为IL-6抑制剂对新冠肺炎患者有益处、部分试验结论为无效,甚至有害。近日世卫组织快速Covid-19疗法证据评估工作组开展系统综述及荟萃研究,考察了IL-6抑制剂与安慰剂或常规治疗相比,对新冠肺炎住院患者28天死亡风险的影响。

研究人员收集了2020年10月至2021年1月间的相关临床试验数据,期间总计27个相关研究纳入本次荟萃分析,随机分为IL-6抑制剂或对照组(安慰剂或常规治疗),除皮质激素外,患者不接受其他免疫治疗药物。研究的主要终点为28天死亡率。
总计10930名患者参与研究,平均年龄61岁,其中女性患者3560名。第28天,IL-6抑制剂组6449名患者中1407人死亡,常规治疗或安慰剂组4481名患者中1158人死亡(OR=0.86)。IL-6抑制剂组患者绝对死亡率为22%,对照组为25%。与对照组相比,托珠单抗治疗后,患者28天死亡风险比值比为0.83,而Kevzara为1.08。与接受了皮质激素治疗的对照组相比,托珠单抗治疗后,患者28天死亡风险比值比为0.77,而Kevzara为0.92。与对照组相比,IL-6抑制剂组机械通气或死亡的风险比为0.77,其中托珠单抗为0.74,而Kevzara为1.00。IL-6抑制剂组28天继发感染率为21.9%,对照组为17.6%。
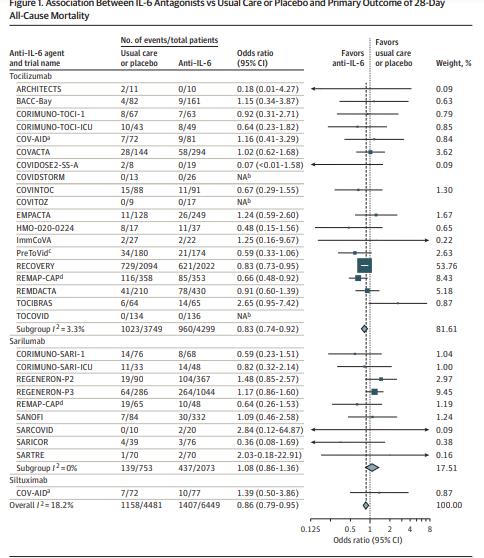
本次荟萃研究证实,新冠肺炎住院患者使用IL-6抑制剂治疗可降低28天死亡风险。
原始出处:
The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association Between Administration of IL-6 Antagonists and Mortality Among Patients Hospitalized for COVID-19 A Meta-analysis. JAMA. July 06,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者死亡#
80
#抑制剂#
64
#死亡风险#
66
#IL-6#
138
#世卫组织#
163
新冠肺炎,疫情何时才能消失
96
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
122
关注患者
139