Drug Dev Ind Pharm:木兰和小蜈蚣在治疗过敏性鼻炎中的药理学机制
2019-06-30 AlexYang MedSci原创
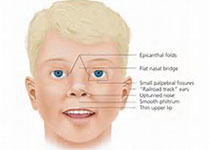
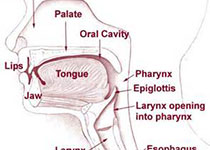
中草药比如木兰花(FM)和小蜈蚣草(CM)在治疗过敏性鼻炎(AR)中是有效的。然而,关于这2种药物同时作用于AR的治疗机制研究很少。最近,有研究人员为了系统的理解这2种药物的同时作用于AR的机制,他们搜索了各种数据库并获得了FM的31种组分和289个靶蛋白,CM的25种组分和465个靶蛋白。研究人员利用Cytoscape-v3. 2. 1软件对FM、CM和AR蛋白的互作网络进行了构建,并利用Ven
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#过敏性#
67
#Pharm#
67
#Drug#
69
#小蜈蚣#
61
#Dev#
77
#IND#
72
#药理学#
67