JAMA Psychiatry:可卡因成瘾机制研究
2015-04-30 赵洲译 MedSci原创
药物成瘾是一种慢性的、复发的脑部疾病,其主要特征就是强迫性寻找和服用药物。作为一个与药物成瘾相关的特征,当服用可卡因时,冲动是一个风险因素且变得更为糟糕。与此相反,强迫性药物使用是这一疾病的主要特征。在可卡因使用者中,冲动和强迫都和不正常的额叶皮质纹状体区结构。大量证据已经证明冲动和强迫在药物成瘾的生理过程中起到了关键性的作用。但脑部网络和成瘾性的关系尚不明确。 为了检验可卡因与纹状体-皮质
药物成瘾是一种慢性的、复发的脑部疾病,其主要特征就是强迫性寻找和服用药物。作为一个与药物成瘾相关的特征,当服用可卡因时,冲动是一个风险因素且变得更为糟糕。与此相反,强迫性药物使用是这一疾病的主要特征。在可卡因使用者中,冲动和强迫都和不正常的额叶皮质纹状体区结构。大量证据已经证明冲动和强迫在药物成瘾的生理过程中起到了关键性的作用。但脑部网络和成瘾性的关系尚不明确。
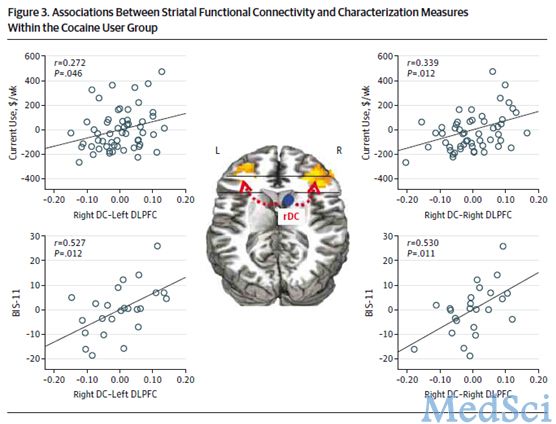
为了检验可卡因与纹状体-皮质通讯干扰有关的假设,研究人员进行了一次案例对照的代表性研究。试验数据在2005年到2011年之间采集的。受试者包括56名可卡因使用者(52人是可卡因依赖、3人是可卡因滥用),另有56人作为对照组(性别、年龄、教育时间、种族、智商和吸烟状态相符)。主要监测指标是两组之间静息状态功能连接强度(rsFC)的差异。在纹状体-皮质循环中,增强的rsFC强度很显著。
研究结果表明,可卡因成瘾和几种具体的纹状体-皮质循环中的受到干扰的rsFC有关。对大脑各个区域的研究为药物成瘾的神经生物学机制提供了新的视角。也为药物成瘾的治疗提供了潜在的新型治疗靶点。这对治疗药物成瘾将有重大的意义。
原始出处:
Hu Y, Salmeron B, Gu H, Stein EA, Yang Y. Impaired Functional Connectivity Within and Between Frontostriatal Circuits and Its Association With Compulsive Drug Use and Trait Impulsivity in Cocaine Addiction. JAMA Psychiatry. Published online April 08, 2015. doi:10.1001/jamapsychiatry.2015.1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#机制研究#
60
#Psychiatry#
64
#可卡因#
82
#可卡因成瘾#
82