盘点:科学家教你如何利用脑洞大开的特技干掉癌细胞
2016-04-22 生物谷 梅斯医学
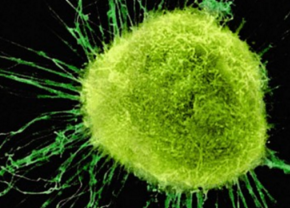
近些年来,随着研究的深入,科学家们在揭示癌症发生机制及耐药的新型通路上取得了突破性的成果,同时科学家也开发出了多种抵御癌症的新型疗法及预防措施,比如我们所熟知的癌症化疗法、放疗法,以及癌症免疫疗法等方法。 而如何靶向杀灭癌细胞呢?科学家们有着不同的方法。近日,发表在国际杂志Cancer Cell上的一项研究论文中,来自卑尔根大学等机构的研究人员发现了一种可以帮助癌细胞扩散的特殊蛋白,那么

近些年来,随着研究的深入,科学家们在揭示癌症发生机制及耐药的新型通路上取得了突破性的成果,同时科学家也开发出了多种抵御癌症的新型疗法及预防措施,比如我们所熟知的癌症化疗法、放疗法,以及癌症免疫疗法等方法。
而如何靶向杀灭癌细胞呢?科学家们有着不同的方法。近日,发表在国际杂志Cancer Cell上的一项研究论文中,来自卑尔根大学等机构的研究人员发现了一种可以帮助癌细胞扩散的特殊蛋白,那么科学家们就找到了癌细胞的致命要害,通过抑制这种特殊蛋白的活性或许就可以抑制癌症扩散,进而杀灭癌细胞。
那么科学家们还有什么高大上的杀灭癌细胞的方法呢?请随小编一一来学习。

伦敦大学学院(UCL)的研究人员已经发现了一种寻找癌细胞的新方法:人体可以寻找肿瘤中的特殊标记来确定肿瘤的位置。它有一个神奇的名字——“阿喀琉斯之踵”。
研究人员相信他们的研究为广大癌症患者们的治疗带来了新的曙光,而且他们的研究有希望在两年内通过测试并广泛应用。研究成果已经在《科学》上发表,该项研究也得到了英国癌症研究院的赞助。
虽然这项研究前景光明,专家们经过评估也说这种方法确实有料,理论依据也很可靠,但这种方法实际上是非常复杂的滴。
原文链接(15 February 2016 doi:10.1038/nnano.2015.343 )
对于那些体内已经存在肿瘤的患者,一般会通过手术切除肿瘤。手术中,医生也想一次清除患者体内的所有癌细胞,但是现实中医生总是处于两难的境地:多切点病灶吧,怕严重损害器官功能;少切点儿吧,残余的癌细胞可能会死灰复燃。其实,医生根本就不知道癌组织与健康组织的界限在哪里。
所以通常在术后,为了巩固手术效果,医生还会根据患者的情况为患者安排化疗或者放疗。但是这种疗法对人体来说会有很大的毒副作用,比较常见的会有脱发、恶心呕吐、食欲不振和白细胞或血小板减少等等,让患者痛不欲生。
说到这里你肯定要问:有没有更好的方法可以为手术治疗兜底的?你肯定知道答案是:有!要不然就没这篇文章了。
美国德州的莱斯大学(Rice University)为这件事情操碎了心。莱斯大学有个研究团队十余年如一日研究一个新项目,意欲把手术后残余的癌细胞一扫光。在这个项目上,他们拼了几代研究僧,发了好多文章。终于发现了一种纳米技术可以帮手术治疗“擦屁股”。

墨尔本的一项药物试验结果喜人,参与试验的大部分癌症患者情况都已好转,甚至有人痊愈。据悉,该试验在Royal Melbourne Hospital和Peter MacCallum Cancer Centre进行,试验中使用的药物名叫Venetoclax,它能够杀死提高癌细胞存活率的BCL-2蛋白质。
面向非常规的癌症试验
这一药物是马克·道森(Mark Dawson)副教授及其团队耗时8年的研究成果。道森是彼得麦克卡伦癌症中心(Peter MacCallum Cancer Cente)癌症表观变化实验室(Cancer Epigenetics Laboratory)的负责人,去年他在接受采访时表示,本次临床实验向所有对常规疗法不抱希望的白血病和多发性骨髓瘤患者换开放,主要目的是找到患者身体所能承受药物剂量的上限。目前药物疗效无法保证,但此次尝试意义重大。"
癌症是世界上最致命的疾病之一,尽管人类已经为之奋战数十年,并取得了较大的进展,但在癌症防治的临床应用上,仍缺少切实有效的新方法。
今年《麻省理工学院技术评论》评选出的亚洲35位35岁以下科技创新精英(TR35)中,有一位叫Majid Ebrahimi Warkiani获奖者,他研发的新技术将为癌症的诊断和治疗带来新的希望。
Warkiani今年32岁,目前是澳大利亚世界顶尖研究型学府新南威尔士大学(UNSW)的助理教授,他还是UNSW纳米医学中心的项目负责人。
Warkiani的新技术叫“透析癌症”(dialysis for cancer),利用这一技术不仅可以发现早期的癌症,评价癌症的治疗效果,以及对癌症的发展做出判断(即所谓的预后);更重要的是,这项技术还有治疗的作用。这种治疗方法简单易懂,就是直接滤掉血液中的癌细胞,延缓甚至阻止癌症的扩散转移。

原文链接(DOI: 10.1007/s13566-015-0239-y)
来自美国休斯顿卫理公会医院的研究人员进行了一项长期临床研究,研究结果表明放射治疗结合"自杀基因治疗"技术可以为前列腺癌病人提供安全有效的治疗。"自杀式基因治疗"技术通过对前列腺癌细胞进行基因修饰使得癌细胞向病人免疫系统发送信号实现"自杀"过程。相关研究结果发表在国际学术期刊Journal of Radiation Oncology上。
共有66名前列腺癌病人参与了1999年到2003年间的II期临床研究,研究人员将参与者分为两组,其中一组病人的肿瘤细胞只存在于前列腺组织,研究人员将该组命名为Arm A,这些病人只接受放射治疗,而另外一组病人携带更具侵袭性的前列腺癌细胞,研究人员将该组命名为Arm B,这组病人要同时接受放射治疗和激素治疗。Arm A组内的病人在研究过程中接受了两次试验性基因治疗,而Arm B组的病人接受了三次基因治疗。
新闻报道:Heat-activated 'grenade' to target cancer
近日在英国利物浦举行的NCRI癌症会议上,有两项新研究开发出了装有热敏触发元件的癌症药物"手榴弹",这项进展能够帮助科学家对肿瘤进行直接的药物靶向治疗。
来自曼彻斯特大学的研究人员之前开发出小的膜泡样脂质体可以用来装载癌症治疗药物并将药物转运到癌细胞内,但是与其他治疗方法所面临的问题相同,如何将脂质体直接导向到肿瘤进行药物投递同时不影响健康组织是这一技术所面临的重要挑战。
最近这两项新研究表明在脂质体上装备热激活触发元件能够部分解决上述问题。研究人员在实验室内对小鼠模型体内的肿瘤进行轻微加热,通过这种方式拉开了"手榴弹"的拉环,实现了对癌细胞杀伤药物的释放并达到靶向癌细胞的目的。

【7】Molecular cell:切断癌细胞备用能源 “饿”死癌细胞
原文链接(doi:10.1016/j.molcel.2015.08.013)
-科学家们通过阻断肺癌细胞对备用营养物质的使用,找到了阻止肺癌细胞生长的新方法。相关研究结果发表在国际学术期刊molecular cell上,这项研究为肺癌治疗提供了新的方向。
癌细胞到底"吃"什么
癌细胞的代谢过程与正常细胞有很大不同。细胞的快速增殖意味着癌细胞对能量的需求会显著增加,而葡萄糖是癌细胞的主要营养来源,它们对葡萄糖的利用速率是正常细胞的几十倍甚至几百倍。但当葡萄糖变得缺乏,癌细胞就必须转而使用备用营养物质以维持细胞生长和存活。
来自加拿大麦吉尔大学,美国华盛顿大学圣路易斯分校,俄罗斯ITMO大学以及英国布里斯托大学的科学家们对葡萄糖供应减少情况下非小细胞肺癌细胞的应答情况进行了研究,结果发现一些肺癌细胞会在葡萄糖缺乏情况下转变它们对"食物"的偏好,转而使用谷氨酰胺。
原文链接(doi:10.1038/ncomms9094)
近日,来自美国的科学家在Nature Communications刊登文章表示,他们开发了一种微笑的植入物,其在小鼠机体中可以扩散到全身来帮助捕捉癌细胞。细胞会随着原始的肿瘤位点而移动进而侵袭其它器官,癌细胞的这一过程被称之为癌症转移,癌症转移往往是在患者晚期阶段被发现,从而导致患者死亡。
而在血液中对循环肿瘤细胞(CTCs)的早期检测或可帮助加速癌症的诊断及疗法的开发;但游动的癌细胞会以很小的数量在机体中“旅游”,而且持续时间较长在其找到新的侵袭位点之前其非常难以发现。这项研究中研究者表示,捕捉CTCs或可帮助抑制癌症转移并且可以有效帮助抑制癌症发展。
美国西北大学的研究者Lonnie Shea教授表示,相比未进行植入物移植的动物而言,接受新型植入物的动物机体肺部的疾病负担明显降低了;实验中研究者开发了一种大约0.5厘米宽的生物可降解的圆盘,并且对每两个小鼠进行植入。这种植入物会利用免疫细胞作为诱饵,同期其还包含有一种扫描仪可以检测到捕获的癌细胞的存在。

【9】Cancer Cell:治疗新潜力药物—让癌细胞“得瑟”而死
原文链接(DOI: 10.1016/j.ccell.2015.07.005)
癌细胞的分裂繁殖速度已经超乎正常,那如果给点刺激,让癌症细胞长得再快点会出现什么情况?——答案是会“得瑟”而死。这种过度刺激肿瘤生长关键蛋白的候选药物或将作为一种新的方法治疗多种癌症。该方法的工作原理是让癌细胞在应激边缘“不堪重负”而死。这篇文章发表在最新的Cancer Cell杂志。
本文资深作者,David Lonard是美国贝勒医学院细胞和分子生物学教授,他表示说:“目前还没有任何被提议或者开发的药物是通过刺激癌基因来达到治疗目的。我们的原型药物能在多种类型的癌症中发挥作用,这将可能作为癌症药物库中新的而更普遍的选择。”
肿瘤细胞需要获得癌基因突变,以支持它们的生长和生存。大量的研究都集中在识别致癌基因,作为癌症药物靶标。致癌基因中,类固醇受体共激活因子(SRC)家族成员尤其具有作为治疗靶标的希望,因为这些蛋白质坐落在使癌细胞快速增长、扩散、并获得耐药性的关键信号传导途径中。在之前的研究中,Lonard和另一位同事Bert O'Malley通过筛选大量的化合物,在动物模型中确定了一种SRC抑制分子,能杀死多种癌细胞,抑制肿瘤生长。这些化合物是类似于常规的抑制癌基因的药物。但是,他们有一个违反直觉的想法:如果他们能破坏关键信号通路,过度刺激SRC,会不会杀死癌细胞?毕竟癌细胞在很大程度上依赖SRC精细调节各种细胞活动,所以SRC刺激可能与SRC抑制在扰乱癌细胞信号活性的平衡一样有效。

原文链接(doi:10.1002/adma.201501803)
刊登在国际杂志Advanced Materials上的一项研究报告中,来自加尼弗尼亚大学的研究人员通过研究开发了一种新型的纳米粒子,其可以在一类特殊蛋白存在的情况下释放药物发挥作用,而特殊蛋白则可以驱动癌症发生转移;文章中研究者开发了一种药物运输系统,其可以有效抑制癌症的发展。
研究者Cassandra Callmann说道,我们以一种小型分子为基础构建了纳米尺度的载体,其可以找到肿瘤并且释放所装载的药物;而这种药物运输系统可以利用一种名为基质金属蛋白酶(MMPs)的特殊酶类蛋白,这种特殊的酶类蛋白在多种癌症中都非常丰富,MMPs可以“撕裂”细胞膜,使得癌细胞可以逃脱而进入机体其他部位引发癌症转移。
研究者开发了一种小型的装载抗癌药物紫杉酚的微型球状结构,并且覆盖以肽类外壳,MMPs可以撕开外壳释放其中所装载的药物,外壳碎片可以形成一种漏网,其就可以包裹药物使其对肿瘤进行稳定地作用。研究者表示,这项研究对于后期开发癌症诊断以及治疗的新型策略非常重要,为了将药物包裹如微型球体结构中,研究者进行了一定的化学处理,事实证明一系列原子对于药物分子的作用效力非常必要,而这也意味着癌症药物在达到肿瘤之前,在其流经的循环系统中是处于失活状态的,这也就避免了药物副作用的发生。

【11】ACSBSE:化疗药物包被或可增强纳米颗粒杀灭癌细胞的效力
原文链接(doi:10.1021/acsbiomaterials.5b00111)
最近,一篇发表于国际杂志ACS Biomaterials Science & Engineering上的研究论文中,来自美国杜克大学的科学家们设计了一种新方法用以开发潜在的纳米癌症疗法;这种方法可以使得水凝胶薄层沉积在纳米壳表面,而这种纳米颗粒仅有100纳米厚,其可以吸收红外线并且产生热量,当其加热时特殊的水凝胶就会失去水分,释放诸如糖类等分子。
文章中研究者将水凝胶沉积于作用肿瘤的纳米壳上,并且以化疗药物涂层覆盖,Jennifer West教授说道,我们的思路是将破坏肿瘤的热疗法同局部药物运输相结合,这种组合拳或是最有效的癌症治疗手段,研究表明许多化疗药物都可以有效作用于发热的组织上,因此将上述两种方法结合或许存在一定的可能性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#脑洞大开#
112
深度好文,值得关注
81
真的长知识啦
131
希望有用
145
原来还有这么多方法
143
说来容易做来难,肿瘤干细胞,如何消灭,应该非常非常困难,它比消灭肿瘤细胞更小了
146
#癌细胞#
56
真的吗?有点不敢相信
82
值得关注
135
不错的文章
110