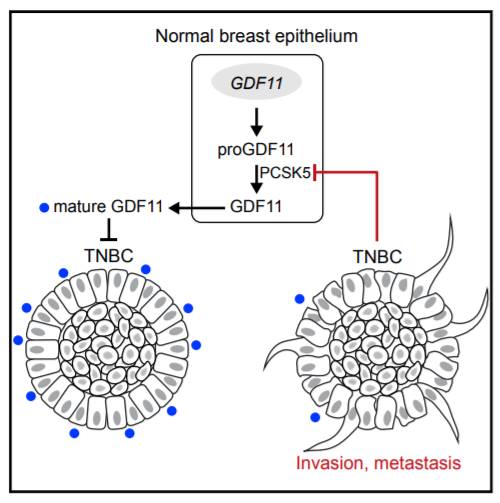
Dev Cell:这种几乎无药可治的乳腺癌,竟然有了新靶点?
2017-11-21 佚名 学术经纬
在乳腺癌里,有一种分类叫做“三阴性乳腺癌”。它并不常见,大概只占乳腺癌总数的10%。但它造成的死亡病例,却占到了乳腺癌患者死亡数的四分之一!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
58
#Dev#
77
#Cell#
72
学习了谢谢分享!!
144
#新靶点#
90
科技的力量是伟大的.难治癌有了新方法.
96