Crit Care:脓毒症或感染性休克患者静脉维生素C治疗的效果分析
2023-03-15 MedSci原创 MedSci原创 发表于上海
在这项荟萃分析中,脓毒症或感染性休克患者的IVVC显著改善了delta SOFA评分,并缩短了血管加压药物使用的持续时间,然而它与短期死亡率的降低无关,并且不良事件风险较高。
脓毒症是一种危及生命的器官功能障碍,与宿主对感染的反应失调有关,脓毒症休克是一种死亡风险较高的脓毒症。这种疾病每年导致全球1100万人死亡,世界卫生组织将其视为一种初级健康威胁。尽管脓毒症在治疗方面取得了重大进展,但除了感染源控制、液体复苏和血管活性药物等基础治疗外,没有足够的证据支持其他治疗方法可提高死亡率,脓毒症幸存者往往会遭受残余器官损伤。因此,寻找有效、安全、经济的辅助治疗方法来降低脓毒症的死亡率和经济负担是非常必要的。
维生素C是一种强大的抗氧化药物,也是休克生存所需的许多生物合成酶的辅助因子,参与内源性抗利尿激素和去甲肾上腺素的合成。近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,该研究旨在更新随机对照试验(RCT)的荟萃分析,并进一步探讨脓毒症或感染性休克患者静脉注射维生素C (IVVC)的结果。

该研究是一项随机对照试验的荟萃分析,研究人员从PubMed、EMBASE和Clinical Trials.gov网站上检索了维生素C治疗脓毒症或感染性休克的随机对照试验(RCT),从数据库创建到2023年1月16日。该研究的主要结果是72-96小时的delta顺序器官衰竭评估(SOFA)评分。两名评审员根据资格标准独立评估RCT:(1)研究类型:RCT;(2)患者人群:≥18岁脓毒症或脓毒症休克患者;(3)干预:与标准治疗相比,任何剂量的IVVC作为单一治疗或与硫胺素或氢化可的松联合治疗,无干预或安慰剂(定义为对照组);(4) RCT描述短期死亡率或SOFA评分。然后,两位作者独立地从RCT中提取相关信息。
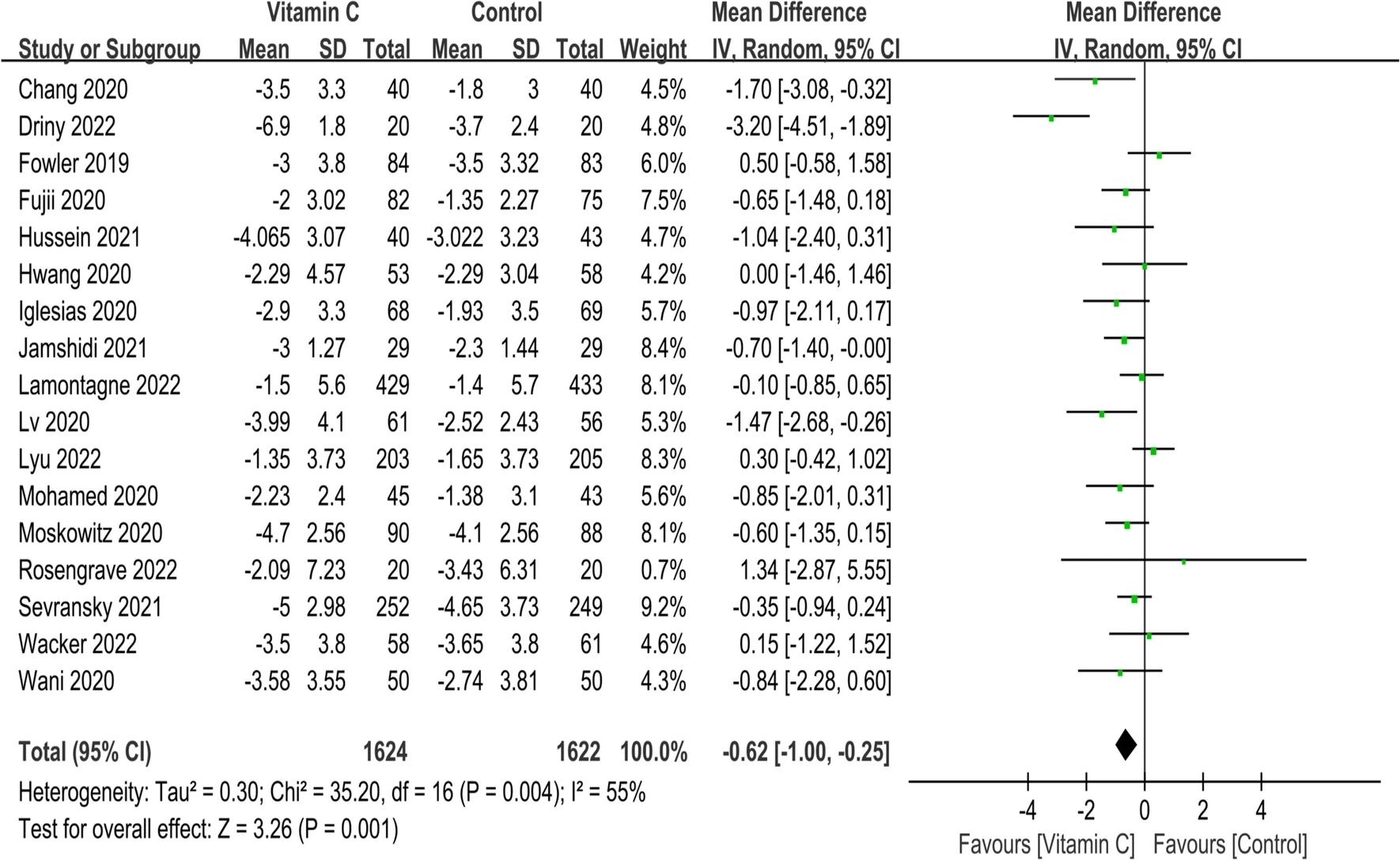
该荟萃分析共确定了18项RCT (n=3364例患者)。从基线到72-96小时,采用IVVC治疗delta SOFA评分(MD为-0.62;95%CI为-1.00至-0.25;p=0.001)和血管加压药物使用时间(MD为-15.07;95%CI为-21.59~-8.55;p<0.00001)有显著影响。IVVC治疗未显示可改善短期死亡率(OR为0.89;95%CI为0.77~1.04;p=0.14);然而,25-100 mg/kg/d剂量组与短期死亡率显著降低相关(OR为0.80;95%CI为0.65~0.97;p=0.03)。IVVC治疗不良事件增加(OR为1.98;95%CI为1.06~3.68;p=0.03)。
由此可见,在这项荟萃分析中,脓毒症或感染性休克患者的IVVC显著改善了delta SOFA评分,并缩短了血管加压药物使用的持续时间,然而它与短期死亡率的降低无关,并且不良事件风险较高。
原始出处:
Baofang Liang.et al.The outcome of IV vitamin C therapy in patients with sepsis or septic shock: a meta-analysis of randomized controlled trials.Critical Care.2023.https://ccforum.biomedcentral.com/articles/10.1186/s13054-023-04392-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












25-100 mg/kg/d剂量组与短期死亡率显著降低相关,最后总结是无关 相矛盾?
64
学习了
54
怎么看?
79
学习了
84
就评论一下 拿个分
75
学习了
86
学了
85
//www.sandwebs.com/article/show_article.do?id=fbf3199815d2 有报道
75
#脓毒症#或#感染性休克#患者静脉#维生素C#治疗的效果分析,这是很多医生喜欢的操作,此前有RCT证实没有明显的效果,未来希望逐步放弃这样的操作了。
0
很好,
73