天疱疮患者的静脉血栓栓塞:一项队列研究
2017-09-12 佚名 CSDCMA皮科时讯论坛
VTE在天疱疮患者中并不罕见,尤其是诊断天疱疮后的第一年。我们必须评估所有天疱疮患者患VTE的风险,尤其住院期间。并对满足要求的患者进行血栓预防治疗。
背景:已有报道静脉血栓栓塞(VTE)是天疱疮患者死亡的一个重要原因。
目的:我们试图评估天疱疮患者VTE的发生率和特征。
方法:回顾性研究172例新诊断的天疱疮患者是否出现VTE。
结果:平均随访4年,10例(6%)患者发生VTE,从诊断天疱疮到出现VTE中位时间为4个月。第一年发生的风险最高,每100个患者年发生5次VTE事件或者第一年VTE风险为5%。 5例患者有深静脉血栓形成,4例有肺栓塞,1例合并上述两种栓塞。年龄和性别与VTE风险无关。大多数患者有患VTE的危险因素,这些因素可能是遗传的或者后天获得的。获得性因素是由于天疱疮治疗及其并发症(包括住院治疗,制动和感染)导致。
局限性:使用现有健康记录限制了对无症状的VTE和VTE危险因素的评估; 没有匹配对照群体的研究。
结论:VTE在天疱疮患者中并不罕见,尤其是诊断天疱疮后的第一年。我们必须评估所有天疱疮患者患VTE的风险,尤其住院期间。并对满足要求的患者进行血栓预防治疗。
关键词:自身免疫性大疱性皮肤病;糖皮质激素; 深静脉血栓形成; 静脉注射免疫球蛋白;天疱疮; 肺栓塞;静脉血栓栓塞。
内容提要
天疱疮患者患静脉血栓栓塞症(VTE)的风险是未知的。
我们发现在患者被诊断天疱疮的第一年VTE发生的风险为5%。大部分VTE发生于危险因素暴露时,如住院治疗、患者制动、感染等。
意识到VTE并采取适当的血栓预防治疗是预防的关键。
天疱疮是一种自身免疫性粘膜皮肤疾病,需长期用免疫抑制性药物治疗。患有天疱疮的患者死亡率增加1,一些队列研究引用静脉血栓栓塞症(VTE)作为天疱疮患者死亡的重要原因2,3。由肺栓塞(PE)和深静脉血栓(DVT)组成的VTE是一种主要的公共健康问题4,它主要发生在住院病人5。并且VTE还是最常见的可预防的住院死因之一6。我们对于天疱疮患者发生VTE的风险知之甚少。在同时诊断为天疱疮和大疱性类天疱疮的住院治疗的患者中发生VTE的风险升高,但天疱疮患者的风险未知7。我们的目的是评估一组队列中天疱疮患者VTE的发病率和特征。
方法
研究设计
在以色列Petah Tikva的拉宾医学中心贝林森医院皮肤科自身免疫性大疱性疾病诊所进行了回顾性队列研究。研究队列是使用的以前的出版物中描述的方案8。简言之,我们诊所在2003年1月1日至2012年12月31日期间诊断出的所有天疱疮患者被列入队列。检查他们的资料来发现是否患有VTE,包括PE和DVT,确定是否患有VTE的手段为计算机断层扫描,血管造影或多普勒超声检查。为进一步证实,查询医院住院病人电脑系统中按国际疾病分类第九修订版诊断为天疱疮合并DVT和P E的患者。提取所有患者的人口统计学和治疗资料。提取VTE病例的获得性和遗传性倾向。
数据分析
通过使用描述统计学总结基线特征,并对数值进行t检验、对比例进行Fisher精确检验。所有分析均采用Stata统计软件(StataCorp 2013,StataCorp LP,College Station,TX)进行。 P<0.05的值被定义为有统计学差异。
结果
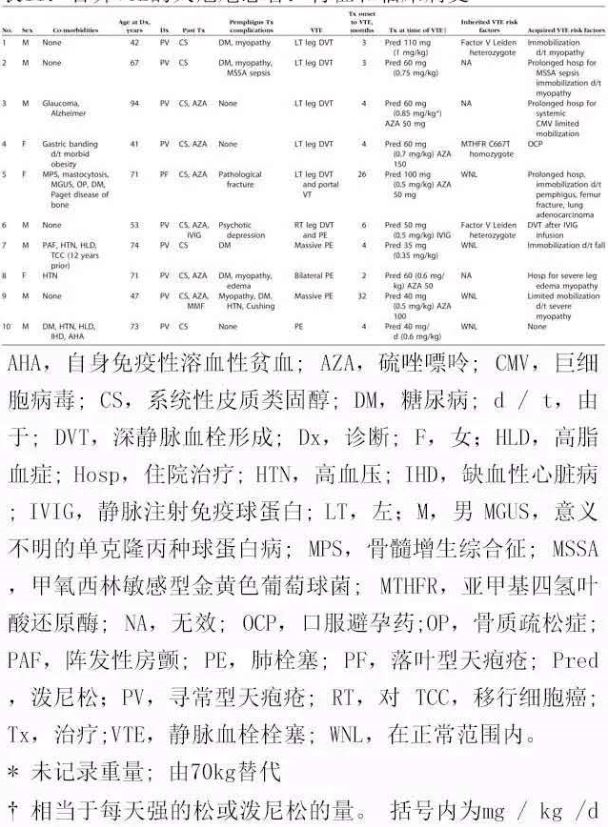
队列包括172例天疱疮患者,平均随访时间为4 ±2.6年。其中153例(89%)有寻常型天疱疮,19例(11%)有落叶型天疱疮。在研究期间,10名患者(6%)发生VTE,从天疱疮诊断到发生VTE时间的中位数为4个月(范围为3-32个月)。通过使用VTE发生人次的方法来计算VTE的风险,我们发现诊断天疱疮后的第一年里发生VTE的风险最高,每100患者年即发生5次VTE事件,转化即得第一年发生VTE的风险为5%。通过VTE分层的患者特征如表I所示。VTE与性别(P = 0.1)、天疱疮诊断时的年龄(P=0.11)或天疱疮类型(P = 0.999)无相关性。VTE病例的详细情况见表II。所有患者均接受平均剂量为62 ±25 mg(0.6 ± 0.2 mg/kg)的泼尼松治疗,5例同时接受硫唑嘌呤、1例同时接受静脉注射免疫球蛋白(IVIG)治疗。7名患者因长期住院治疗和制动等天疱疮治疗并发症而获得了VTE危险因素。3名患者有遗传性VTE危险因素。2名患有重度PE和血液动力学障碍的患者在重症监护病房住院治疗,1例患者患有轻度肺动脉高压。其他人都完全康复。
讨论
VTE给普通群众造成了重大疾病负担,每年每1000人中VTE发病率为0.75至2.699。在住院患者中,已有报告发病率高达1.3%(DVT)和0.4%(PE)10。在一项大的队列研究中,我们发现诊断天疱疮后第一年发生VTE的风险为5%。虽然我们没有将这种风险与匹配的对照组的风险进行比较,但这本身就是一个很重要的数据,因为VTE是导致致残率和死亡率的重要原因4。
表Ⅰ :患或不患静脉血栓栓塞症的天疱疮患者的特征
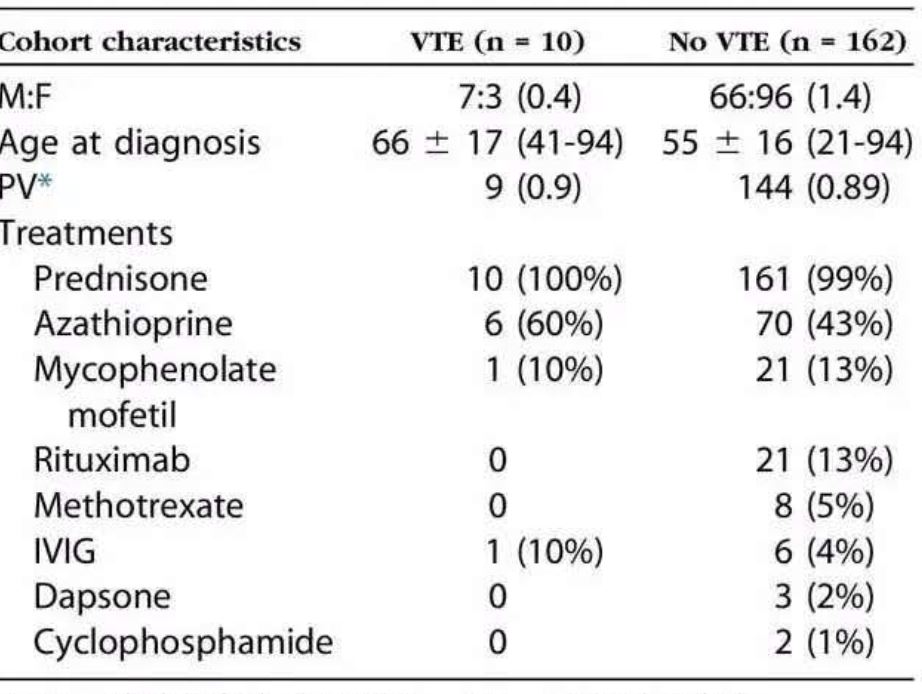
IVIG静脉注射免疫球蛋白,PV,寻常型天疱疮;VTE经脉血栓栓塞症.
表Ⅱ:合并VTE的天疱疮患者:特征和临床病史
天疱疮患者患VTE中有几种可能的原因。住院治疗是VTE的独立危险因素11,当天疱疮患者患有基础疾病3或有治疗相关并发症时发生VTE也比较常见8。实际上,4名被研究的患者在发生血栓时正住院治疗并发症。制动也可能易患VTE,其相关机制较多,包括系统应用皮质类固醇(CS)诱导的肌病,继发于CS诱导的骨质疏松或维生素D缺乏的病理性骨折,以及严重的衰弱性感染。急性感染在天疱疮中频繁发生8,它可增加VTE的风险13。比如,我们发现金黄色葡萄球菌败血症和全身巨细胞病毒感染已被报道可增加发生VTE的风险14。CS治疗是天疱疮的主要治疗方法,但它能通过增加纤维蛋白原和凝血因子的水平增加VTE的风险15。PE的风险高于DVT,这可能解释了为什么当DVT通常更普遍时,我们观察到PE仍与DVT一样多16。一名患者在接受IVIG治疗的同时发生了DVT,即使已知这是非常罕见17的治疗并发症18。该患者是因子V Leiden的杂合子,但是IVIG可能增加了遗传性VTE风险19。天疱疮对VTE的发展起到主要作用(如果有的话),但不清楚。有证据表明VTE在越来越多的自身免疫性疾病中的风险增加20。一些风险与疾病特异性因素相关,如狼疮中的心磷脂抗体。自身免疫性疾病也可能因为全身炎症而使其有血栓形成的倾向,可能是通过上调促凝血因子,抑制抗凝血因子和抗纤维蛋白溶解作用促进血栓形成20。然而,我们并未发现在天疱疮患者中血浆凝血酶原,D-二聚体和血清组织因子的水平有升高21,这强调天疱疮和血栓形成之间的关系需要进一步的的研究。
天疱疮患者患VTE的风险引发了通过药物手段(如抗凝剂),机械手段(例如间歇气压)或下腔静脉过滤进行血栓预防的各种问题。这种风险必须与这些措施的并发症(如出血)进行权衡,特别是长期服用CS药物的患者可能需要相应胃肠道预防。对于住院病人,临床指南可以帮助决定是否进行血栓预防治疗22。指南将患者分为血栓形成低风险低与高风险组,仅推荐高风险组进行血栓预防。估计血栓形成的基线风险是基于风险评估模型,如Padua预测评分23,根据明确的的临床因素进行风险分层。基于Padua评分,我们的研究中有3/4的住院患者需要血栓预防,但这部分患者并未接受血栓预防治疗。住院患者血栓预防使用不足并不是我们的队列研究中独有的问题,而是整个世界范围内的问题24,这导致许多卫生机构将促进血栓预防作为患者安全策略的首要任务4,25。对门诊进行血栓预防更为复杂,缺乏指导决策的指南。在获得更多数据之前,必须按照具体情况对天疱疮患者患VTE风险与其预防血栓并发症的风险进行比较。
我们的研究有几个局限性。它受限于仅使用现有的健康记录,这限制了我们可以评估的VTE风险因素。我们确定了在完全证实患有天疱疮患者群体中VTE的发病率; 然而,没有对照群体,我们无法报告VTE在天疱疮患者中的相对风险。对不同群体的另外的研究可以提高我们的结果的普遍性。如果患者在外院接受治疗,并且如果小的无症状VTE未被诊断,那么我们可能会低估VTE的数量。但更高的VTE发病率只会进一步支持本研究的结论。
在这项关于大量天疱疮患者VTE的研究中,我们发现当天疱疮治疗及其并发症越多时,天疱疮诊断后第一年患者发生VTE的风险最高。皮肤科医生必须了解这种风险,并酌情提供血栓预防治疗。关于疾病特异性的危险因素对整体VTE风险的贡献还须进一步研究。
使用到的缩写:
CS: 糖皮质激素
DVT: 深静脉血栓
IVIG: 静脉注射免疫球蛋白
PE: 肺栓塞
VTE: 静脉血栓栓塞
参考文献略。
原始出处:
Snyder KE1, Barger MM,et al.Identification as Gifted and Implicit Beliefs About Intelligence: An Examination of Potential Moderators. J Adv Acad. 2013 Nov;24(4):242-258.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#静脉血#
71
#静脉#
65
学习.谢谢分享
88
谢谢分享.学习了
91
好好学习.多看看
109
谢谢分享学习了
105
学习了谢谢作者分享!
94