Eur Heart J:心血管疾病患者超加工食品摄入量与全因和特定原因死亡的关系
2021-12-01 MedSci原创 MedSci原创
富含UPF的饮食与既往有心血管事件的个体全因死亡和CVD死亡风险增加相关,这可能是由于肾功能改变所致。UPF摄入量增加是CVD二级预防中的一个主要的公共卫生问题。
超加工食品(UPF)已经在世界范围内变得越来越普遍。 如果日常饮食中,UPF占比较高、大量食用,不仅会增加各种不良健康状况,如肥胖、心血管疾病以及癌症等, 据报道,UPF与心血管疾病以及全因死亡风险增加有关。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估有心血管疾病(CVD)病史的个体中UPF摄入量与死亡率之间的关联,并分析一些可能将UPF摄入量与死亡联系起来的生物学分子机制。

研究人员对在Moli-sani研究(2005-2010期间,意大利)中招募了1171名伴有CVD病史的男性和女性(平均年龄为67±10岁),并进行了纵向分析,受试者随访了10.6年(中位数)。研究人员使用食物频率问卷评估了受试者的食物摄入量。UPF是根据加工程度使用NOVA分类进行定义的,并根据UPF(g/天)与总食物消耗量(g/天)之间的比率(%)的四分位数进行分类。在反事实框架内,研究人员使用Logistic回归模型评估了18种炎症、代谢、心血管和肾脏生物标志物的介导作用。
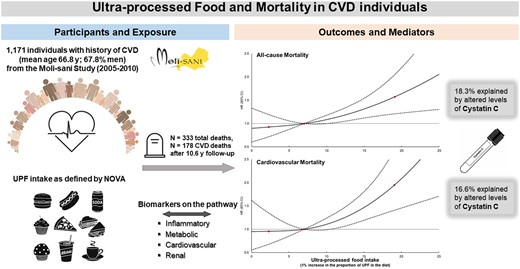
在多变量调整的Cox分析中,与最低摄入量(Q1,UPF<4.7%)相比,较高的UPF摄入量(Q4,≥11.3%)与更高的全因风险(风险比[HR]:1.38;95%置信区间(CI):1.00-1.91)和CVD死亡(HR为1.65;95%CI为1.07-2.55)相关。研究人员还观察到了UPF摄入量每增加1%与全因死亡率和CVD死亡率之间呈线性的剂量-反应关系。胱抑素C水平的改变分别解释了UPF(饮食中摄入量增加1%)与全因死亡率和CVD死亡率之间相关性的18.3%和16.6%。
由此可见,富含UPF的饮食与既往有心血管事件的个体全因死亡和CVD死亡风险增加相关,这可能是由于肾功能改变所致。UPF摄入量增加是CVD二级预防中的一个主要的公共卫生问题。
原始出处:
Marialaura Bonaccio,et al.Ultra-processed food intake and all-cause and cause-specific mortality in individuals with cardiovascular disease: the Moli-sani Study.European Heart Journal.2021.https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehab783/6446064?redirectedFrom=fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#疾病患者#
76
#摄入量#
78
学习了
134
#ART#
81
#血管疾病#
178
#HEART#
87
太给力啦,非常有用
130
学习啦
107
学习啦
134
很好的研究
115