Int J Rheum Dis:儿童期发病的系统性红斑狼疮的生存率的影响因素有哪些?
2015-12-26 phylis 译 MedSci原创
背景:儿童期发病的系统性红斑狼疮(cSLE)占的SLE患者的15-20%。尽管一些研究报道成人SLE预后,鲜有对中东地区cSLE的调查研究。方法:这项回顾性的研究,招募1992年到2011年患有系统性红斑狼疮的孩子。记录和分析疾病开始时间点的临床和实验室数据。应用Kalpan-Meier计算生存率。应用Cox回归分析评估死亡的预测因子。结果:研究期间,招募了188名诊断为SLE的儿童。9名患者排除
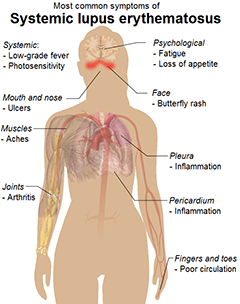
背景:儿童期发病的系统性红斑狼疮(cSLE)占所有SLE患者的15-20%。尽管一些研究报道cSLE预后,但鲜有对中东地区cSLE的调查研究。
方法:这项回顾性的研究,招募1992年到2011年患有系统性红斑狼疮的孩子。记录和分析疾病开始时间点的临床和实验室数据。应用Kalpan-Meier计算生存率。应用Cox回归分析评估死亡的预测因子。
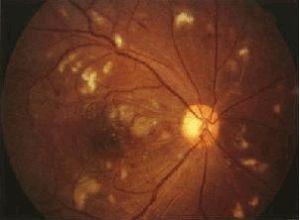
结果:研究期间,招募了188名诊断为SLE的儿童。9名患者排除统计,因随访失访(6)和数据不完整(3例)。疾病开始时,患者年龄的平均年龄为14.4(3.05)岁。仅仅22名(11.8%)10岁前发病。总之,20名患者(11%)死亡,这些孩子都在10岁以后。最常见的死亡原因是狼疮性肾炎(10例,50%死亡),其次是感染(35%)、脑血管意外(10%)及肺泡出血(5%)。5年、10年、15年、20年的累积生存率分别为91%、87%、85%和79%。多变量分析中,SLE发病时有血尿或胸膜炎与生存呈负相关。
结论:在伊朗cSLE生存率与其他发展中国家相似。基线出现血尿可增加cSLE患者的死亡率。未来可进行大样本的前瞻性试验,研究cSLE的其他方面。
原文出处:
Fatemi A, Matinfar M, et al. The association between initial manifestations of childhood-onset systemic lupus erythematosus and the survival. Int J Rheum Dis. 2015 Dec 3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
61
#Dis#
60
#生存率#
65
#狼疮#
55
#红斑#
68
#影响因素#
50