Lancet Neurol:卒中后晚发性癫痫发作风险“SeLECT”先知
2018-04-11 贾朝娟 环球医学
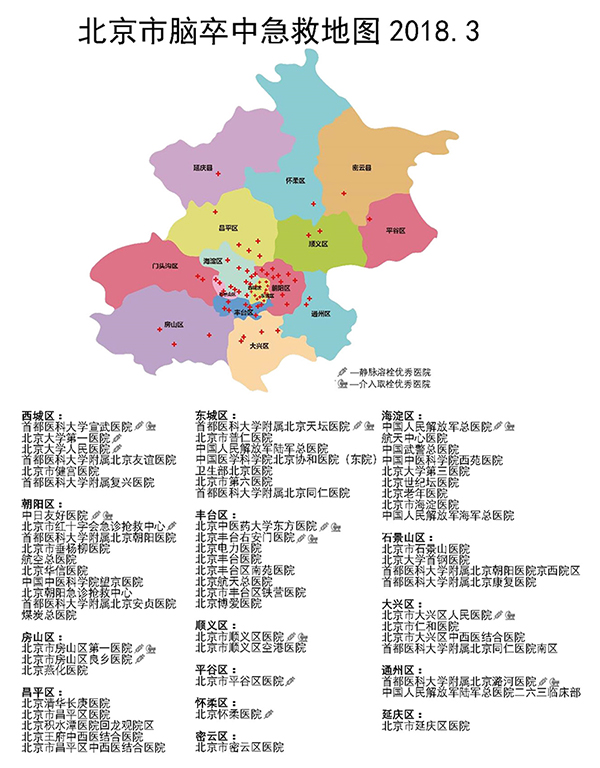
脑卒中是成人癫痫发作最常见的病因,并且可加重卒中风险,影响卒中的预后和患者的生活质量,甚至威胁生命。通常卒中和第一次迟发性癫痫之间有数周至数年的潜伏期。过去十年动物模型抗癫痫药物研发结果显示,脑卒中后的最初几周内,需要在癫痫发作接踵而至之前进行早期干预。但既往所有在人中进行的防止卒中后癫痫发作治疗相关研究均不成功。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
74
#卒中后#
58
#SeLECT#
67
#Lancet#
58
好文献.学习了
81
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
91
hbjjj
81
认真学习.不断进步.把经验分享给同好.点赞了!
88