【一般资料】
男,26岁
【主诉】
10d前无明显诱因出现右侧肢体麻木,以右上臂、右大腿麻木感较重。
【现病史】
外院MRI示:左侧丘脑占位性病变,胶质瘤可能性偏大,不排除淋巴瘤。2d前病人劳累后出现头部胀痛,以双颞侧为重,遂就诊于深圳市第二人民医院。
【体格检查】
四肢肌张力正常,双侧肢体肌力Ⅴ级,右侧上、下肢触觉、痛温觉减退,以右上肢、右大腿明显。
【辅助检查】
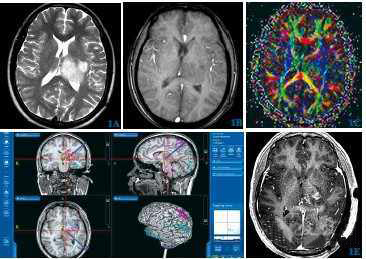
MRS:兴趣区取病灶及对侧正常对比区,谱线示病灶内谱线异常,Cho峰较对侧正常区域增高,NAA峰较对称区域明显降低,Cho/NAA比值均较正常区域升高,Cho/Cr值明显升高。DTI:右侧丘脑-基底核区及左颞部纤维稍减少,对应FA值较正常减低,ADC值较正常增高。
【初步诊断】
结合MRI平扫+增强,考虑左侧丘脑占位性病变,胶质瘤可能性偏大,不排除淋巴瘤。
【治疗】
手术及病理所见:导航引导下于左侧顶上小叶造瘘,大小约3cm,纵向切开脑皮质3cm见肿瘤,肿瘤质地较软,呈鱼肉状,颜色为暗红色,血供较丰富,切取稍许瘤组织送冰冻,冰冻结果考虑胶质瘤。显微镜下沿着肿瘤肉眼边界,进一步分离肿瘤,内侧到侧脑室枕角,上界达中脑外侧,显微镜下切除鱼肉状肿瘤成分,瘤腔创面予速即纱和明胶海绵填塞,生理盐水冲洗干净。免疫组化显示:Ki-67=15%、GFAP、Olig-2、Vim、P53阳性,IDH1、R132H阴性。病理结果:符合多形性黄色星形细胞瘤(WHOⅡ级),灶性区域为间变性多形性黄色星形细胞瘤(WHOⅢ级)。分子病理示:MGMT甲基化阴性,IDH1野生型,IDH2野生型。术后给予替莫唑胺放化疗。术后4个月随访,复查头颅MRI增强扫描,左侧丘脑占位术后改变,未见肿瘤复发,查体:病人右侧肢体肌力4级,右侧肢体麻木症状较术前好转,KPS评分大于90分。
【讨论】
丘脑多形性黄色星形细胞瘤为WHOⅡ级,属胶质瘤的一种,发病率较低。多形性黄色星形细胞瘤好发于儿童和年轻人,10~19岁为高发年龄,目前多认为其起源于多潜能神经干细胞。本例病人影像学表现:肿瘤实质性部分在CT上表现为低密度;MRI上T1表现为低或等信号,T2表现为等或稍高信号,增强后可见实质性肿瘤及瘤结节强化;MRS上Cho峰较对侧正常区域增高,NAA峰较对称区域降低。根据影像学检查结果,考虑该病人为胶质瘤,多形性黄色星形细胞瘤可能性较大。完善术前准备,利用导航确定肿瘤位置,在电生理监测下避开顶上小叶功能区,选择手术入路,手术切除过程中轻柔操作,减少对正常脑组织的骚扰,电生理监测预防重要神经功能损伤,沿脑皮质自然间隙分离至肿瘤组织后,静脉注射荧光素钠,调节蔡司显微镜至荧光功能,反复在显微荧光下观察肿瘤细胞密集区域,给予切除,在切除大部分肿瘤后再次用导航棒定位,探查有无肿瘤残余及肿瘤切除边界。术后结合免疫组化与分子病理结果,以及本例病人病理结果:灶性区域为间变性多形性黄色星形细胞瘤(WHOⅢ级),考虑病人属丘脑高级别胶质瘤。根据临床统计学资料,考虑愈后较差,所以肿瘤全切,是决定病人术后5年生存率的关键。本例病人起病早期是因肿瘤压迫内囊后肢出现临床症状就诊,术后4个月随访,复查头颅MRI增强扫描,未见肿瘤复发,查体:病人右侧肢体肌力4级,右侧肢体麻木症状较术前好转,KPS评分大于90分。所以对于丘脑胶质瘤,肿瘤全切对于病人的愈后起决定作用。但因随访时间短,病人长期预后及放化疗对病人的治疗价值,还有待进一步观察,该手术开颅后随着脑脊液的释放,脑组织出现漂移,神经导航定位会出现偏差,因本院无术中磁共振,缺乏术中指导,实现术中导航下切除肿瘤技术需进一步完善。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#多形性#
74
深部的pxa第一次见到.学习
93
#细胞瘤#
70
#丘脑#
57
#丘脑#
61
学习.谢谢分享.
94