JAHA:贫血的老年人卒中后死亡风险更高
2016-08-18 fsy 译 MedSci原创
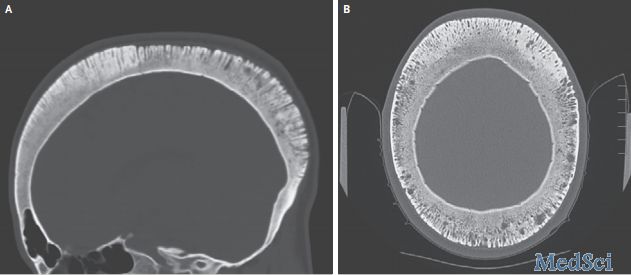
根据美国心脏协会杂志的最新研究,美国心脏协会/美国卒中协会杂志的一项新的研究显示,贫血,缺乏红细胞,可能与患中风的老年人的死亡风险更高的风险有关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#卒中后#
98
学习了,文章有深度,值得探究。
80
很好,不错,以后会多学习
102
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
113
#死亡风险#
72
#AHA#
56
值得学习
95