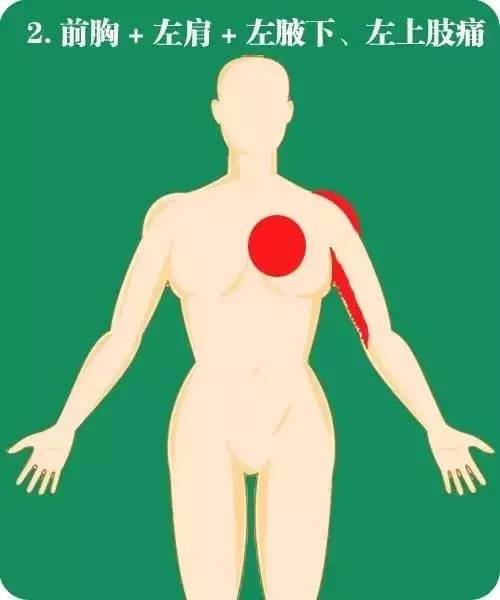
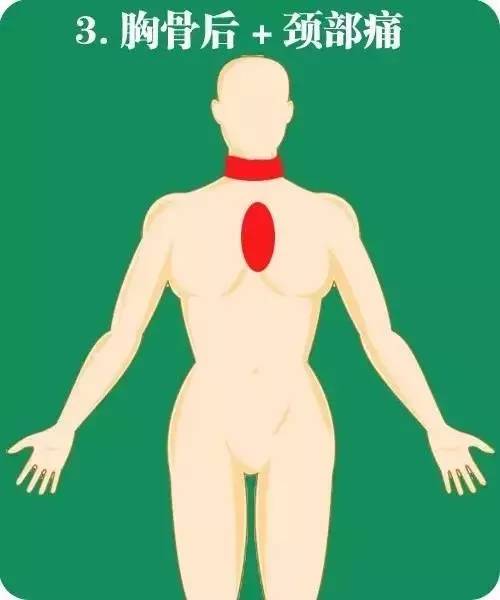
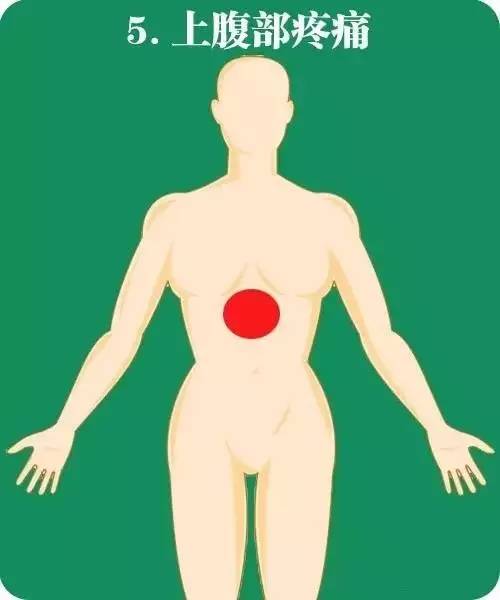
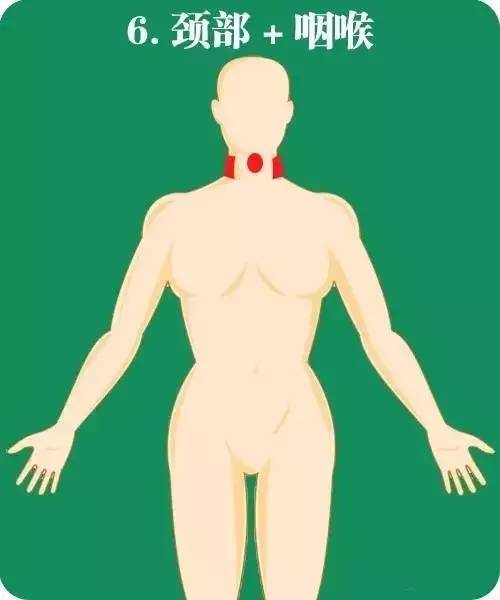
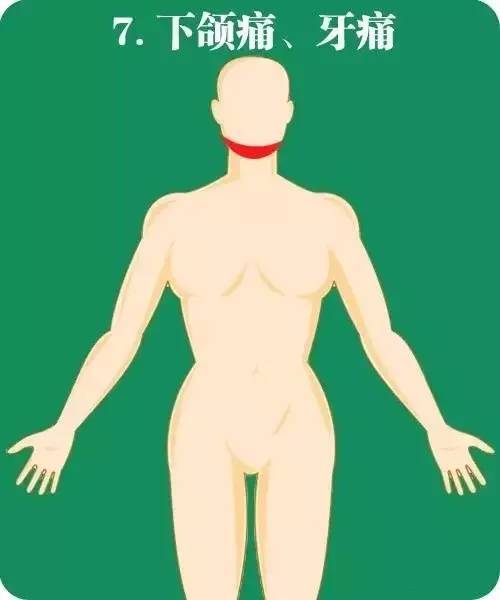
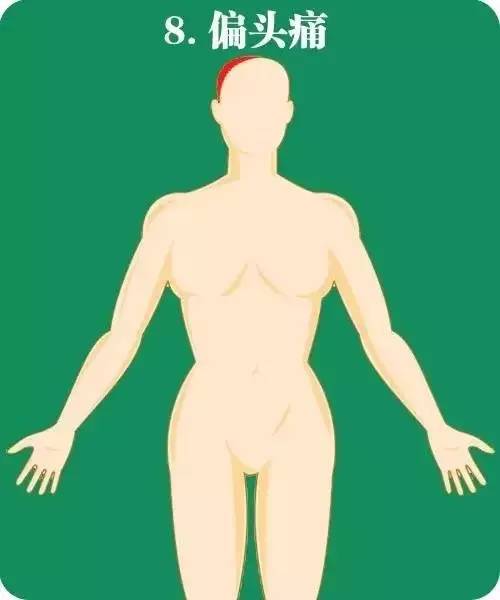
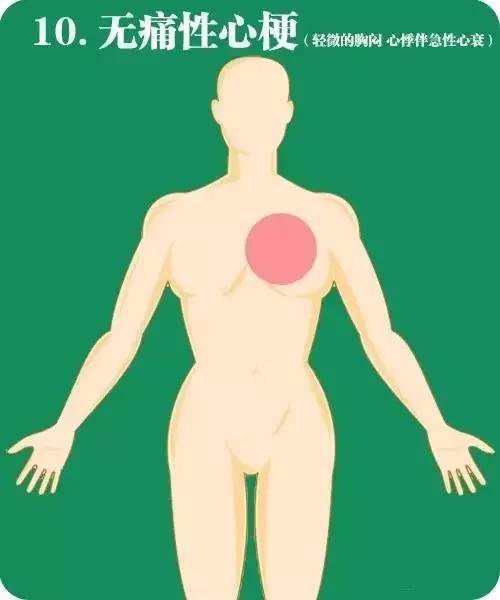
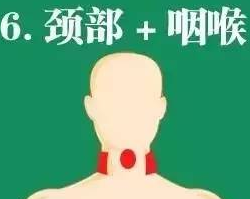
图解:急性心梗的10个疼痛部位
2015-12-15 佚名 医学之声
急性心肌梗死疼痛的部位在心前区和或胸骨后,但也有一些不典型的疼痛部位值得警惕。 众所周知,急性心肌梗死疼痛的部位在心前区和或胸骨后,表现为突发性胸骨后或心前区压榨性剧痛,可放射至左颈根部、背部或左上肢,持续半小时以上,休息和舌下或口服硝酸甘油无效,常伴有烦躁不安、出汗、恐惧或有濒死感,不敢继续工作或活动。 但有20%~30%的病人症状不典型,首发症状表现为胸外非典型部位疼痛,这种情况极
急性心肌梗死疼痛的部位在心前区和或胸骨后,但也有一些不典型的疼痛部位值得警惕。
众所周知,急性心肌梗死疼痛的部位在心前区和或胸骨后,表现为突发性胸骨后或心前区压榨性剧痛,可放射至左颈根部、背部或左上肢,持续半小时以上,休息和舌下或口服硝酸甘油无效,常伴有烦躁不安、出汗、恐惧或有濒死感,不敢继续工作或活动。
但有20%~30%的病人症状不典型,首发症状表现为胸外非典型部位疼痛,这种情况极易忽视,导致误诊或漏诊。当有急性心梗高危因素的患者,突发下面这些部位的疼痛应该警惕AMI可能。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











配图很喜欢,精明,好理解!
161
简明…
202
图不错,
150
文章
113
赞!
189
赞一个,
125
不错的文章!
107
了解了,
128
已经收藏…
108
好文章,值得看。
128