Evolution:禁食疗法弊端再添新证据
2014-07-21 佚名 生物谷
纵观历史,人们一直在寻找长生不老之法,不管是从饮食还是服用维生素药片上,人们尝试了很多种方法;如今,来自英国巴斯大学的研究人员通过研究表示,抗老化疗法比如服用抗氧化剂或限制饮食等仅对抗衰老具有短暂的效应,而且其也存在一定的风险,相关研究刊登于国际杂志Evolution上。近年来,一种名为间歇性禁食(Intermittent Fasting)或者5:2饮食的一种策略广为流行,名人和媒体都认为这种饮食
纵观历史,人们一直在寻找长生不老之法,不管是从饮食还是服用维生素药片上,人们尝试了很多种方法;如今,来自英国巴斯大学的研究人员通过研究表示,抗老化疗法比如服用抗氧化剂或限制饮食等仅对抗衰老具有短暂的效应,而且其也存在一定的风险,相关研究刊登于国际杂志Evolution上。[pdf free]
近年来,一种名为间歇性禁食(Intermittent Fasting)或者5:2饮食的一种策略广为流行,名人和媒体都认为这种饮食方式可以降低血压、增加机体寿命以及保护机体抵御各种疾病,比如痴呆症等。
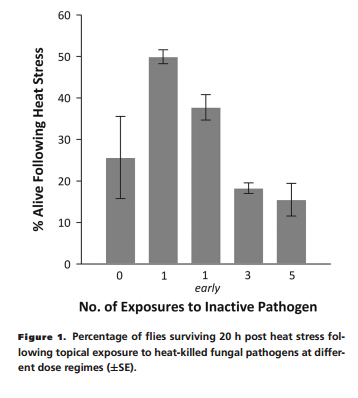
然而本文中,研究者认为这样的饮食方式或许会长期影响机体的免疫系统,使得人们对感染更加敏感;研究者在果蝇机体中研究了4种压力和免疫相关的基因,这几个基因被认为与长寿相关,并且可以帮助理解预期寿命和抵御感染能力之间的关系,相似的基因也会被抗老化疗法(比如绝食疗法或服用抗氧化剂)激活。
未来研究者们还将通过对果蝇模型进行深入研究来揭示高蛋白饮食,比如阿特金斯饮食法是否会增加果蝇机体的免疫系统功能。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了有用。
114
#Evolution#
64
#食疗#
54
#Evolut#
64
为什么不注明作者?
171