Nature:重大突破!30年来首次提出治疗肾结石的新方法
2016-08-10 佚名 生物谷
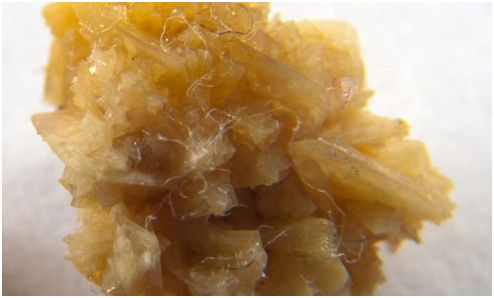
在一项新的研究中,研究人员发现证据证实一种天然的水果提取物能够溶解草酸钙晶体,即人肾结石中最为常见的组分。这一发现可能导致人们30年来首次在治疗草酸钙结石中取得进展。相关研究结果于2016年8月8日在线发表在Nature期刊上,论文标题为“Molecular modifiers reveal a mechanism of pathological crystal growth inhibition
这项研究提供首个证据证实化合物羟基柠檬酸(hydroxycitrate, HCA)是一种有效地抑制草酸钙晶体生长的物质,而且在某些条件下,实际上能够溶解这些晶体。研究人员也解释了它是如何发挥作用的。
Rimer说,这些发现是实验研究、计算研究和人体研究结合在一起的结果。
肾结石是在肾脏内形成的小的坚硬的矿物质沉积物,影响着高达12%的男性和7%的女性。高血压、糖尿病和肥胖能够增加这种风险,而且报道的发病率也在上升。
在过去三十年来,对肾结石的预防治疗并没有发生太多变化。医生们告诉有风险患上结石的病人喝大量的水,并且避免吃富含草酸盐的食物,如大黄、秋葵、菠菜和杏仁。他们经常推荐服用柠檬酸盐(citrate, CA),以柠檬酸钾的形式,即一种能够延缓草酸钙晶体生长的补充剂,但是一些人不能够忍受它产生的副作用。
Asplin指出HCA是一种可能的治疗选择。HCA在化学结构上类似于CA,而且也能够作为一种膳食补充剂加以使用。
研究人员写道,“HCA有望作为一种阻止肾结石的潜在疗法。在治疗上,HCA可能比CA(以柠檬酸钾的形式)更好。”
同时对CA和HCA的研究发现尽管这两种化合物抑制草酸钙晶体的生长,但是HCA更加强效,而且表现出有利于开发新疗法的独特性质。
研究人员随后利用原子力显微镜(AFM)研究了草酸钙晶体在真实的生长条件下与CA和HCA之间的相互作用。根据Rimer的说法,这种技术允许他们实时地在近分子分辨率下记录晶体生长。
论文第一作者、在Rimer实验室从事研究的休斯顿大学研究生Jihae Chung注意到当草酸钙晶体接触到特定浓度的HCA时,这些AFM显微图片记录到这种晶体确实在缩小。Rimer怀疑这个初步的发现是异常的,这是因为在高度过饱和的溶液中观察到这种晶体在溶解是非常罕见的。在文献中报道的最为有效的抑制剂仅仅是阻止这种晶体生长。
结果表明Chung的初步发现是正确的。一旦研究人员证实在过饱和溶液中溶解草酸钙晶体是可能的,他们就研究了解释这种情形为何发生的原因。
来自美国匹兹堡大学的Giannis Mpourmpakis和他的研究生Michael G. Taylor利用密度泛函理论(density functional theory, DFT)---一种高度准确的计算方法,被用来研究材料的结构和性质---解决HCA和CA如何结合到钙和草酸钙晶体上。他们发现HCA与草酸钙晶体表面更强地结合在一起,产生一种张力,而且这种张力似乎通过钙离子和草酸根离子的释放得到缓解,从而导致晶体溶解。
HCA也在人受试者体内进行测试。7个人在三天内服用这种补充剂,这就允许研究人员确定HCA通过尿液排泄出来,这也是这种补充剂作为一种疗法发挥作用所必需的。
Rimer说,尽管这项研究为设计一种有效的药物奠定基础,但是问题仍然存在。他说,长期安全性、剂量和进一步的人体临床试验还是需要的。
他说,“但是我们初步的发现是非常大有希望的。如果它在体内发挥作用,就像我们在实验室中开展的临床试验那样,那么HCA有潜力降低慢性肾结石病患者的发病率。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
59
#新方法#
54
被题目吸引!
92
这都行,不是研究大病才能发文章
102
重大突破
80
学习学习!
102