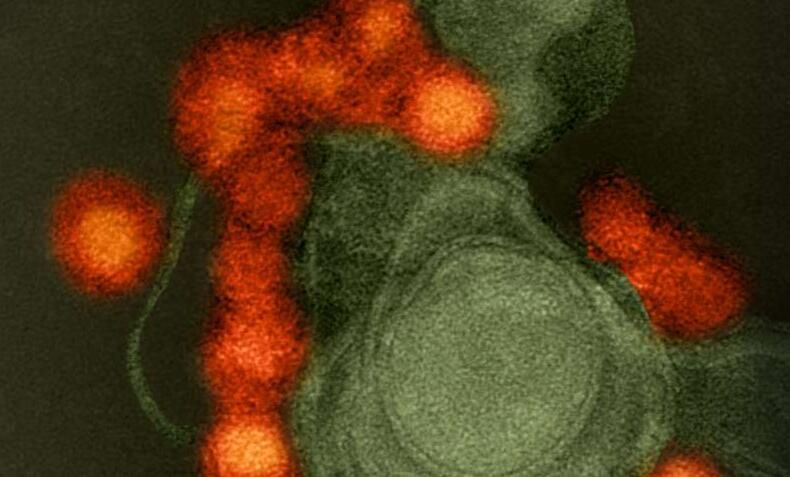
Sci Transl Med:高福院士揭示寨卡病毒治疗性抗体的机制
2017-02-10 MedSci MedSci原创
中科院微生物研究所严景华研究员与高福院士近期合作揭示高效、特异性人源寨卡病毒(zika virus, ZIKV)治疗性抗体及其机制。研发寨卡病毒治疗性抗体方面取得重要进展,率先找到高效、特异性人源寨卡病毒(zika virus, ZIKV)治疗性抗体及其机制,该抗体在小鼠模型上能有效治疗ZIKV感染,有望成为治疗其感染的候选药物。随着研究的深入,ZIKV的危害逐渐被揭示,从最初的发烧、皮疹等轻
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Transl#
51
#TRA#
53
#寨卡病毒#
51
#寨卡#
59
#Med#
52
最新研究进展
84
不错,学习了
86