Circulation:STEMI患者的补氧,是好还是坏?
2015-06-11 李妍 cmt
澳大利亚一项研究显示,对于不存在组织缺氧的STEMI患者,补氧疗法可增加早期心肌损伤,且与6个月时心肌梗死面积增大相关。论文5月22日在线发表于《循环》(Circulation)杂志。研究纳入经12导联心电图诊断为STEMI的患者638例,比较吸氧(8 L/min)和不吸氧对患者的影响。研究主要终点为通过心肌酶、心肌肌钙蛋白(cTnI)和肌酸激酶(C
澳大利亚一项研究显示,对于不存在组织缺氧的STEMI患者,补氧疗法可增加早期心肌损伤,且与6个月时心肌梗死面积增大相关。论文5月22日在线发表于《循环》(Circulation)杂志。
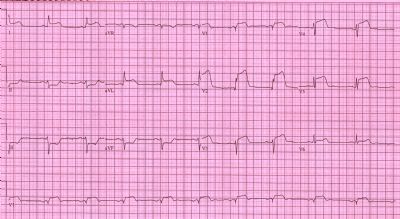
研究纳入经12导联心电图诊断为STEMI的患者638例,比较吸氧(8 L/min)和不吸氧对患者的影响。研究主要终点为通过心肌酶、心肌肌钙蛋白(cTnI)和肌酸激酶(CK)评估的心肌梗死面积。共441例患者完成主要终点分析。次要终点包括心肌梗死复发、心律失常和6个月时由心脏磁共振(CMR)成像评估的心肌梗死面积。
结果为,吸氧与不吸氧组cTnI平均峰值相当(P=0.18)。与不吸氧组相比,吸氧组CK平均峰值显著增加(P=0.01);心肌梗死复发率显著增加(P=0.006);且心律失常发生频率增加(P=0.05)。6个月时,吸氧组经CMR评估的心肌梗死面积增加(P=0.04)。
STEMI患者的补氧问题——依然悬而未决
美国波士顿大学医学院佐伦·尼德尔科维奇(Zoran S. Nedeljkovic)和埃利斯·雅各布斯(Alice K. Jacobs)指出,对于STEMI患者实施氧疗,美国心脏病学会和美国心脏学会(ACC/AHA)指南的推荐意见不断在变化。1999年,指南建议,对肺充血和动脉血氧饱和度<90%的患者给予氧疗(Ⅰ级推荐);对于无并发症的急性心肌梗死患者,在最初2~3小时内常规给予氧疗(Ⅱa级推荐)。2004年,指南建议,对组织缺氧(动脉血氧饱和度<90%)或肺充血患者在最初6小时内持续给予氧疗(Ⅰ级推荐)。然而,2013年的指南指出,几乎没有证据支持或反对在STEMI急性期常规给予氧疗,故未就此给出推荐意见。
很多人认为氧疗是一种相对良性的治疗。然而,将近40年前的一项随机对照研究显示,常规吸氧对于无并发症的心肌梗死患者无益甚至可能有害。近年来的一些研究也对常规补氧提出了质疑。氧疗所致的不良效应可能与冠脉阻力增加及生成活性氧有关。
本研究为无组织缺氧患者常规实施氧疗相关质疑又提出了新证,且研究的多中心随机设计以及严谨全面的数据分析增加了研究结果的可信性。尽管吸氧和不吸氧组在梗死相关动脉(infarct-related artery)方面的差异并不显著,但两组患者的缺血危险区(area at risk)存在明显差异。尽管成功的经皮冠状动脉介入治疗(PCI)和血流量的恢复对患者预后非常重要,但这种缺血危险区的差异亦可能导致最终梗死面积的差异。
基于现有证据,仅建议对于存在组织缺氧或明显肺充血的急性STEMI患者,在接受PCI前给予补氧。未来需要更大型的研究,证明对于无组织缺氧的STEMI患者,氧剥夺是否会影响其临床转归。
原始出处:
Nedeljkovic ZS1, Jacobs AK2.O2 for STEMI: Still Up in the Air.Circulation, May 22, 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









常规低流量…
137
#STEMI患者#
47
看看
157
#STEM#
54
学你了
163
也许,常规的处理里面有些错误没意识到。可以有更多研究来论证效果。
78
现在对于STEMI,医院都常规吸氧。
179
值得进一步研究
102
实验出真理
86
ROS?
119