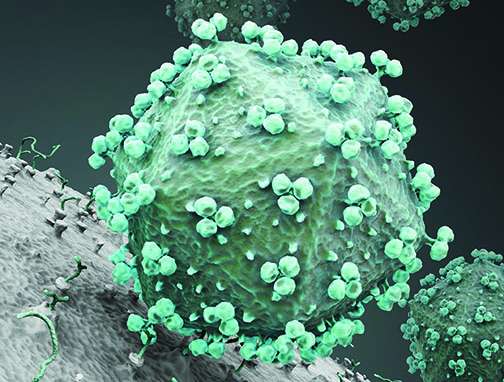
Clin Infect Dis:HIV的母婴传播更容易发生在哪类人身上?
2017-06-23 sunshine2015 来宝网
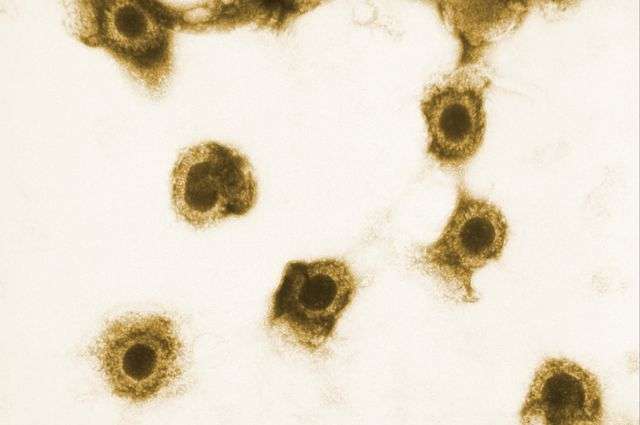
艾滋病病毒感染(HIV)阳性,在分娩时的尿液中存在巨细胞病毒或CMV的女性,比没有巨细胞病毒或CMV的HIV女性传播HIV给子女的可能性高5倍。加州大学洛杉矶分校牵头了这项研究。该研究发现,这些女性将巨细胞病毒传染给婴儿的可能性高30倍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Dis#
86
#母婴#
54
学习了
102
不错的文章,值得推荐
102
洁身自好,爱护自己保护孩子
108