Cell Metabolism:高胰岛素水平可导致肥胖
2012-12-20 Cell Metabolism 互联网 liuygi
一个意外的发现表明,某些有关健康饮食的普遍的想法可能是错误的,实际上却能导致人们体重增加。 这个发现来自一位来自英国的哥伦比亚大学的研究人员,并被发表在《细胞代谢》杂志上。 该研究起初是观察胰岛素的作用的试验,胰岛素是一种激素,能使机体储存血糖以便作为能量以后使用。胰岛素缺乏能导致糖尿病,而且,根据同杂志发表的一项不同研究,胰岛素主要作用受损,可能引起无限制的脂肪分解,而更严重地,这将导致2型
一个意外的发现表明,某些有关健康饮食的普遍的想法可能是错误的,实际上却能导致人们体重增加。
这个发现来自一位来自英国的哥伦比亚大学的研究人员,并被发表在《细胞代谢》杂志上。
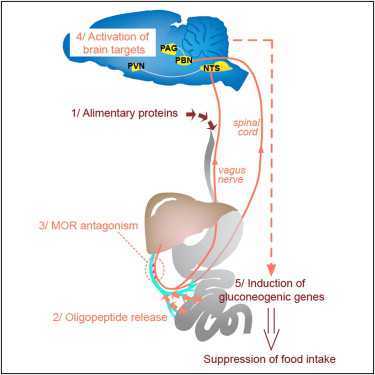
该研究起初是观察胰岛素的作用的试验,胰岛素是一种激素,能使机体储存血糖以便作为能量以后使用。胰岛素缺乏能导致糖尿病,而且,根据同杂志发表的一项不同研究,胰岛素主要作用受损,可能引起无限制的脂肪分解,而更严重地,这将导致2型糖尿病。
细胞生理学副教授詹姆斯.约翰逊在分析了动物体内胰岛素的作用后,发现过多的胰岛素可能是有害的。
约翰逊将小鼠分成两组,两组都喂给高脂饮食。一组为对照组,由正常小鼠组成,另一组由被培育为仅有半数胰岛素的小鼠组成。
结果显示,正常小鼠超重,这就像科学家所预料的。然而,低水平胰岛素小鼠体重并没有增加,这是由于它们的脂肪细胞代谢了更多的能量,而使储存变少了。依然很瘦的小鼠没有变胖,并能更健康地生活。
这意味着,依据约翰逊的发现,高脂饮食所引起的正常小鼠额外增加的胰岛素导致了肥胖。换言之,和人一样,小鼠或许产生了过多的胰岛素。
该研究表明,人们能通过时常地将胰岛素水平带回到健康所需的最小量来维持一个健康体重。这可以通过增加两餐间隔时间和不吃零食,不在进餐时间过度饮食。
一般的认为,为了保持苗条,人们每天应该吃少量食物,但在这项研究中显示,这是无效的。
约翰逊结论
“胰岛素对储存血糖很重要,它也能将好事变成坏事。如果我们能将胰岛素水平维持在敲到好处,我们将扭转肥胖的高发,肥胖是许多疾病的一个危险因素,如糖尿病、心脏疾病和癌症。”
胰岛素和肥胖之间的关系令人惊讶
鉴于UBC生命科学研究所约翰逊并没有实施检测肥胖的研究,因而他对他的发现感到相当惊讶。他最初着手确定,是否胰腺β细胞(胰岛素分泌细胞)因本身的胰岛素分泌被促进增加了。
约翰逊的两个发现时意料之外的:
l低胰岛素小鼠不增加体重
l这些小鼠中多数(甚至显着降低胰岛素水平)仍然没有发展成糖尿病
根据2007-2009年测量的身高和体重数据,估计加拿大每4个人中就有1个是肥胖的。从1981年到2007-2009年,在几个年龄段中,男性和女性的肥胖率增加了两倍。
虽然,有药物能限制胰岛素,并防止人们增加体重,但它们的副作用却抵消了用药的优势。因此,需要做更多的研究,以便能发现阻止人们产生额外的胰岛素或者改变对特异靶组织影响的药物。
与胰岛素相关的拓展阅读:
- Cell Metabolism:高胰岛素水平可导致肥胖
- 病例:二甲双胍联合胰岛素治疗的时机与获益
- 2型糖尿病患者胰岛素治疗结构化管理模式研究:一项开放、多中心、前瞻性RCT研究
- LRP16基因对胰岛素分泌和胰岛素抵抗的影响
- FDA支持新型超长效德谷胰岛素上市 更多信息请点击:有关胰岛素更多资讯

DOI:10.1016/j.cmet.2012.10.019,
PMC:
PMID:
Hyperinsulinemia Drives Diet-Induced Obesity Independently of Brain Insulin Production
Arya E. Mehran1, 2, Nicole M. Templeman1, 2, G. Stefano Brigidi1, Gareth E. Lim1, 2, Kwan-Yi Chu1, 2, Xiaoke Hu1, 2, Jose Diego Botezelli1, 2, Ali Asadi1, 2, Bradford G. Hoffman2, Timothy J. Kieffer1, 2, Shernaz X. Bamji1, Susanne M. Clee1, James D. Johnson1, 2
Hyperinsulinemia is associated with obesity and pancreatic islet hyperplasia, but whether insulin causes these phenomena or is a compensatory response has remained unsettled for decades. We examined the role of insulin hypersecretion in diet-induced obesity by varying the pancreas-specific Ins1 gene dosage in mice lacking Ins2 gene expression in the pancreas, thymus, and brain. Age-dependent increases in fasting insulin and β cell mass were absent in Ins1+/−:Ins2−/− mice fed a high-fat diet when compared to Ins1+/+:Ins2−/− littermate controls. Remarkably, Ins1+/−:Ins2−/− mice were completely protected from diet-induced obesity. Genetic prevention of chronic hyperinsulinemia in this model reprogrammed white adipose tissue to express uncoupling protein 1 and increase energy expenditure. Normalization of adipocyte size and activation of energy expenditure genes in white adipose tissue was associated with reduced inflammation, reduced fatty acid spillover, and reduced hepatic steatosis. Thus, we provide genetic evidence that pathological circulating hyperinsulinemia drives diet-induced obesity and its complications.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
71
#Meta#
67
#MET#
73
#Cell#
52
#胰岛#
64
#Metabolism#
69
#ABO#
59