Semin Arthritis Rheum:RA患者结核感染后可否继续使用生物制剂
2017-05-27 佚名 结核帮
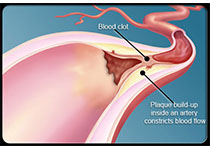
肿瘤坏死因子拮抗剂(TNFi)目前用于治疗许多慢性炎症性疾病,包括类风湿关节炎(RA),强直性脊柱炎,银屑病关节炎等。TNFi 对细胞内细菌感染(如结核杆菌)的免疫应答起着关键作用。已有研究显示,接受 TNFi 治疗的风湿病患者结核感染风险增加 0.6 至 24.1 倍。 对于已有结核感染的 RA 患者是否能继续使用 TNFi 这个问题,韩国学者 Cho 等给出了答案,结果发表在近期的杂志 Sem

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#生物制剂#
60
#结核感染#
75
#Arthritis#
50
#结核#
69
#ART#
0
学习了,又涨知识了!
86