Nat Commu:器官移植排斥反应可能不是永久性!
2015-07-10 佚名 生物谷
近日,来自美国芝加哥大学的研究人员在国际学术期刊Nature Communication在线发表了一项最新研究进展,他们发现器官移植过程中免疫耐受的存在并非永久性,在已经形成免疫耐受的病人体内还可能再发生免疫排斥,但不会形成永久性的免疫记忆,而调节性T细胞在免疫耐受形成过程中发挥重要作用。器官移植是治疗器官衰竭的一种重要方法,进行了器官移植的病人往往需要终身服用免疫抑制药物,也有一些病人可以经过一
近日,来自美国芝加哥大学的研究人员在国际学术期刊Nature Communication在线发表了一项最新研究进展,他们发现器官移植过程中免疫耐受的存在并非永久性,在已经形成免疫耐受的病人体内还可能再发生免疫排斥,但不会形成永久性的免疫记忆,而调节性T细胞在免疫耐受形成过程中发挥重要作用。
器官移植是治疗器官衰竭的一种重要方法,进行了器官移植的病人往往需要终身服用免疫抑制药物,也有一些病人可以经过一些诱导产生免疫耐受,其移植器官可以在不服用免疫抑制药物的情况下被机体所接受,但即使已经存在长时间的免疫耐受,一些类似于细菌感染的事件仍会触发宿主免疫系统对移植器官产生排斥反应。
进行该项研究的研究人员在之前的工作中发现,细菌感染触发的对移植器官的排斥反应会引起大量免疫细胞靶向移植器官,干扰小鼠对移植器官的耐受性,但令人吃惊的是,这些细胞在排斥反应产生七天后会显著减少,这一现象与非耐受性移植受体产生的排斥反应大不相同,在非耐受性移植受体体内这些靶向移植器官的免疫细胞始终维持较高水平。
在该项研究中,研究人员对实验小鼠模型进行了心脏移植,并诱导宿主产生免疫耐受。在形成稳定耐受两个月后,通过细菌感染触发宿主对移植心脏产生免疫排斥反应。随后,研究人员在排斥反应产生一周之后,又用与第一个供体基因相同的供体心脏进行了第二次心脏移植,结果第二个移植心脏被宿主顺利接受,在整个研究期间维持正常功能。在另外一组实验中,研究人员在免疫排斥反应产生一个月之后进行了第二次心脏移植,结果类似。
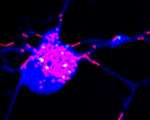
随后,研究人员发现调节性T细胞在免疫耐受重建过程中发挥重要作用。他们在进行第二次心脏移植前一天移除宿主小鼠的调节性T细胞,结果新的移植心脏受到宿主的排斥,这些结果表明,调节性T细胞在阻止其他免疫细胞产生排斥反应的过程中扮演了"刹车"的角色。
总得来说,这项研究的结果表明已经形成免疫耐受的器官移植病人在发生免疫排斥反应之后可以通过短期免疫抑制药物进行治疗以保护移植器官,免疫耐受会在一段时间之后重新恢复。这项研究对于器官移植的临床应用具有一定意义。
原始出处:
Michelle L. Miller, Melvin D. Daniels, Tongmin Wang, Jianjun Chen, James Young, Jing Xu, Ying Wang, Dengping Yin, Vinh Vu, Aliya N. Husain, Maria-Luisa Alegre & Anita S. Chong.Spontaneous restoration of transplantation tolerance after acute rejection.Nature Communications, July 7, 2015.doi:10.1038/ncomms8566
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
61
看看
134
#排斥#
58
#排斥反应#
54
看看
166