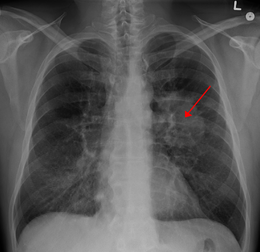
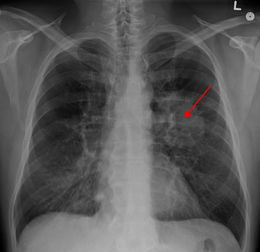
JCO:年龄对Ⅲ期非小细胞肺癌同步放化疗疗效的影响
2017-05-19 MedSci MedSci原创
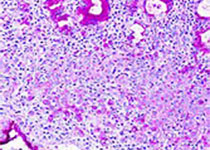
肺癌是美国死亡率第一的肿瘤,其中大部分患者为非小细胞肺癌。同步放化疗是治疗Ⅲ期非小细胞肺癌的标准治疗方式。年龄较大的患者副反应出现的可能性更高,在同步放化疗中的受益更少。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCO#
69
#Ⅲ期非小细胞肺癌#
72
#非小细胞#
55
#放化疗#
47
#同步放化疗#
68
不错,学习了!!
94
学习了,很好
71
同步放化疗毒性较大,身体状况不好的患者较难承受
84
学习了,感谢分享
86
学习,感谢分享
74