J Am Heart Assoc:巨噬细胞NCOR1缺陷或可改善心肌梗死和血管内膜新生的情况
2021-07-09 MedSci原创 MedSci原创
NCOR1(核受体核心压迫因子1)是基因转录的一个重要核心调节因子。已有研究表明,巨噬细胞中的NCOR1在代谢调节中发挥重要作用。然而,巨噬细胞NCOR1在应对心肌梗死(MI)或血管损伤中的功能还没有
NCOR1(核受体核心压迫因子1)是基因转录的一个重要核心调节因子。已有研究表明,巨噬细胞中的NCOR1在代谢调节中发挥重要作用。然而,巨噬细胞NCOR1在应对心肌梗死(MI)或血管损伤中的功能还没有被阐释。
本文中,研究人员利用巨噬细胞NCOR1基因敲除小鼠,结合小鼠MI模型,证明巨噬细胞NCOR1的缺失能明显减少梗死面积,改善MI后的心脏功能。此外,巨噬细胞NCOR1的缺乏明显抑制了动脉线损伤小鼠模型中的新内膜增生和血管重塑。该研究结果已发表于J Am Heart Assoc。

MI和动脉线损伤后,巨噬细胞NCOR1基因敲除小鼠的心脏和动脉中炎症和巨噬细胞增殖显著减弱。来自巨噬细胞Ncor1基因敲除小鼠的培养的原代巨噬细胞在白细胞介素-1β、白细胞介素-6或脂多糖刺激时表现出较低水平的炎症基因表达,同时炎症信号级联的激活也较少,包括信号转导和转录激活因子1以及核因子-κB。此外,与对照组细胞相比,巨噬细胞Ncor1基因敲除的巨噬细胞在培养中的增殖能力大大降低,其细胞周期进程受到抑制。
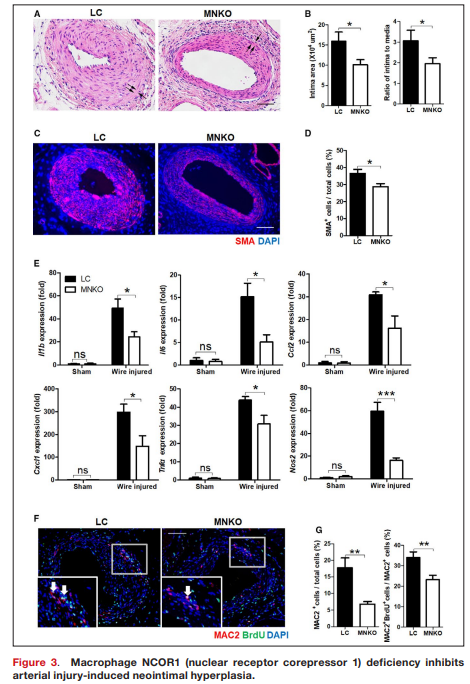
总之,该研究结果表明,NCOR1是巨噬细胞炎症和增殖的一个关键调节器,巨噬细胞中NCOR1的缺失会减弱MI和新内膜增生。因此,巨噬细胞NCOR1可作为MI和再狭窄的潜在治疗靶点。
原始出处:
Lin-Juan Du, et al., Macrophage NCOR1 Deficiency Ameliorates Myocardial Infarction and Neointimal Hyperplasia in Mice. J Am Heart Assoc. 2020 Aug 4;9(15):e015862. doi: 10.1161/JAHA.120.015862.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#内膜#
76
#ART#
64
#HEART#
92
谢谢分享
96