Blood:FcRn可放大IgG免疫复合物对组织因子活性的诱导
2020-03-21 MedSci原创 MedSci原创
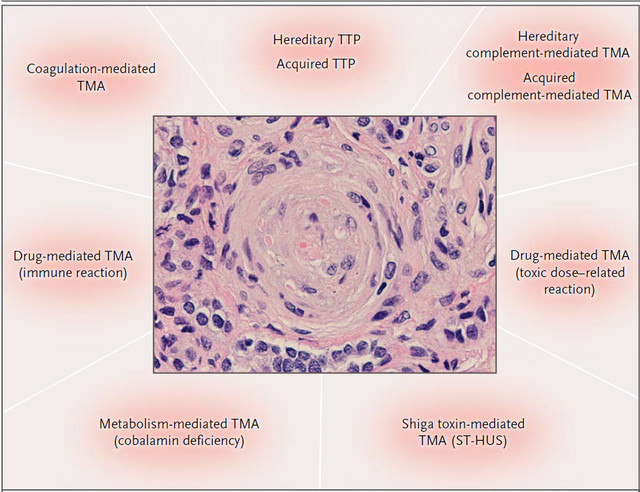
新生的IgG Fc受体,FcRn,参与包含IgG的免疫复合物介导的组织因子活性的诱导。抑制FcRn或可减轻由包含IgG的免疫复合物所介导的疾病患者的血栓形成前表现。
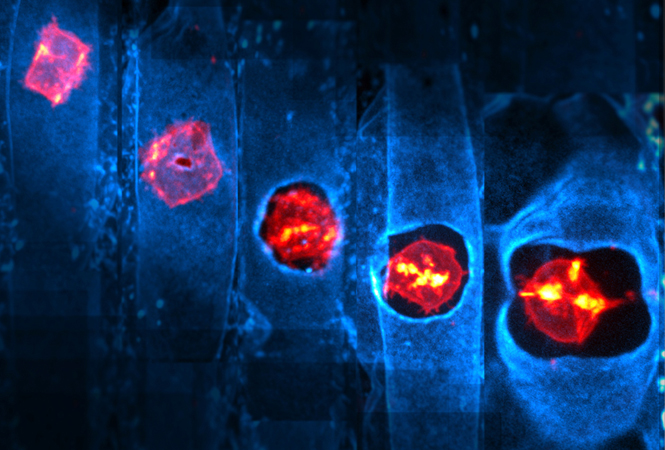
介导IgG和白蛋白循环的新生Fc受体(FcRn)也参与对含IgG的IC的细胞反应。FcRn是否也参与THP-1单核细胞和人单核细胞通过IgG-ICs所介导的TF依赖性Xa因子活性的诱导?研究人员对此进行研究。
包含抗血小板因子F(PF4,与肝素诱导性血小板减少症[HIT]相关)的IgG抗体、b-2-糖蛋白-1(与抗磷脂抗体综合征[APS]相关)或红细胞的抗α-Rh(D)抗体(介导体内溶血)的ICs所介导的Xa因子活性诱导可被人源化单克隆抗体(MoAb)抑制,该抗体可阻断IgG与人FcRn结合。
与FcγR和FcRn结合的IgG ICs诱导Xa因子活性,而Fc被改造后的IgG-ICs不能与FcRn结合,也不能诱导Xa因子活性。在表达人FcgRIIa的HIT转基因小鼠模型中,注射α-FcRn MoAb可防止微血管损伤后纤维蛋白沉积。
本研究结果表明FcRn具有可溶性和细胞相关性含IgG的IC诱导的TF依赖性FXa活性。目前,在热自身免疫溶血性贫血的临床试验中,FcRn抗体可降低IgG抗体和含IgG的ICs,还可以降低静脉血栓栓塞的风险。
原始出处:
Douglas B. Cines, et al. FcRn augments induction of tissue factor activity by IgG-containing immune complexes. Blood. March 18, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复合物#
84
#CRN#
78
#组织因子#
62
#FcRn#
70
#免疫复合物#
69
#IgG#
102