NEJM:支气管黑色素瘤-病例报道
2018-11-15 xing.T MedSci原创
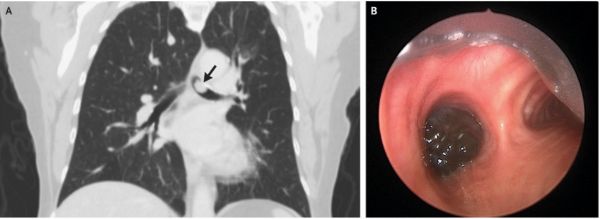
体格检查发现左肺明显的吸气和呼气喘鸣。胸部计算机断层扫描显示息肉样病变,并且阻塞左主干支气管。硬性支气管镜检查发现支气管中移动性色素沉着肿块。用电烙套管和氩等离子体凝固清除肿块。肿块的病理检查证实了转移性黑素瘤的诊断,伴有BRAF突变。
患者为一名70岁的女性,因进行性呼吸急促,且对支气管扩张剂无反应2个月而到呼吸科门诊就诊。在就诊前三年,她的左肩部切除了黑色素瘤。当时淋巴结清扫的结果发现转移为阴性。
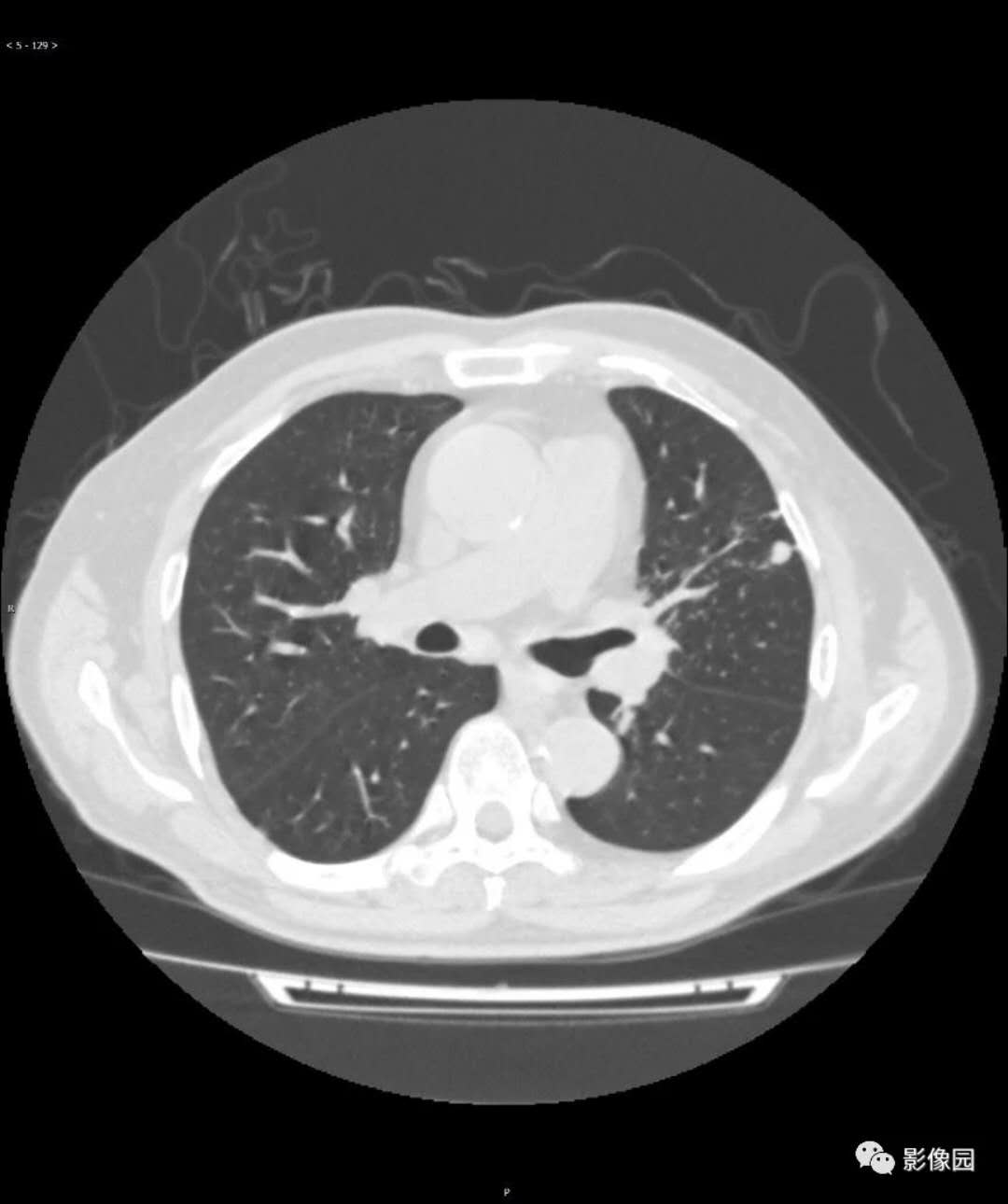
体格检查发现左肺明显的吸气和呼气喘鸣。胸部计算机断层扫描显示息肉样病变,并且阻塞左主干支气管(如图A箭头所示)。硬性支气管镜检查发现支气管中移动性色素沉着肿块(如B组所示)。用电烙套管和氩等离子体凝固清除肿块。肿块的病理检查证实了转移性黑素瘤的诊断,伴有BRAF突变。
肿瘤切除后,患者的喘息和呼吸短促症状完全消退,并开始接受曲美替尼和达拉菲尼联用治疗黑素瘤。
原始出处:
Christopher Manley,et al. Melanoma in the Bronchus.N Engl J Med 2018;https://www.nejm.org/doi/full/10.1056/NEJMicm1805380
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#支气管#
81
#色素#
84
#黑色素#
73
#黑色素#
146